INTRODUCTION
Pneumocephalus usually results from trauma, neoplasms, infections, and surgical interventions12). Barotrauma-induced pneumocephalus resulting from a rapid change in the surrounding pressure is a major concern for airline passengers and scuba divers5,6,9-11,14).
Recent advances in aircraft technology have led to a tremendous increase in air travel for the general population and for neurosurgical patients.
Neurosurgical procedures, including cranial and spinal surgery, could be a cause of residual intracranial air and could create a dormant fistulous tract that opens when the cabin pressure changes.
During air travel, a neurosurgical patient could experience fatal tension pneumocephalus resulting from expansion of residual air in the head and pneumoencephalomeningitis secondary to cerebrospinal fluid (CSF) leakage and the backflow of contaminated air through the bony defect.
To generate interest and considerations about safe air travel of neurosurgical patient among practicing consultant neurosurgeons, the authors report a rare case of barotrauma-induced pneumocephalus experienced by a high risk patient after commercial air travel.
CASE REPORT
A 49-year-old female presented to the emergency department with a severe headache, nausea, and vomiting after one hour flight on a domestic commercial airliner. Her mental status was alert without confusion. A cranial nerve examination revealed anosmia through both nostrils and a visual field defect of the left inferior homonymous quadranopsia. Additional cranial nerve function, motor and sensory function, the deep tendon reflex, and cerebellar function were normal.
Ten years ago, this patient was diagnosed with meningioma in the occipital lobe and underwent a suboccipital craniotomy to remove the tumor at another hospital. Further questioning revealed that the patient underwent four additional otolaryngologic operations (two operations involving the mastoid sinus and two involving the frontal skull base through the nose) to manage CSF rhinorrhea four years after initial the craniotomy. The patient did not know the precise cause of the CSF leak. Finally, a lumboperitoneal shunt was placed, and the patient did not experience further symptoms of a CSF leak. The revision surgery for a recurrent tumor was performed last year; at the time of the incident discussed here, the patient was returning home after gamma knife radiosurgery for the residual tumor.
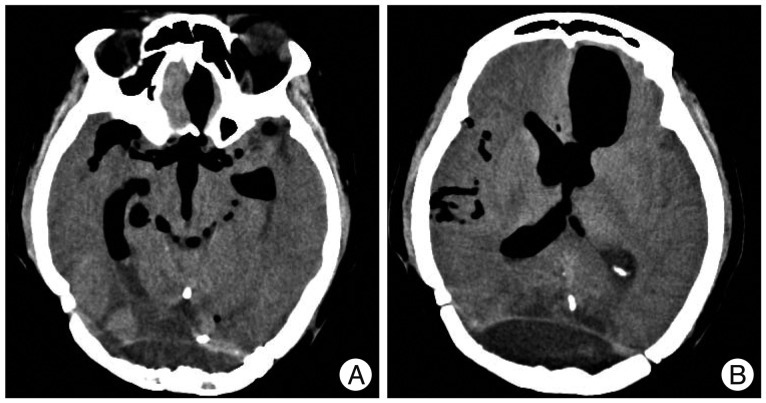
A computed tomography (CT) scan of the head (Fig. 1) demonstrated extensive air within the subarachnoid space of the basal cistern, bilateral lateral and third ventricle, and extending to the intraparenchymal portion of the left frontal lobe.
The routine laboratory blood tests (leukocyte count, hemoglobin, hematocrit, glucose, blood urea nitrogen, creatinine, sodium, potassium, chloride, and C-reactive protein) were normal.
Normal saline and analgesics were administered via an intravenous line, and a gradual resolution of the headache was achieved within several days. Seven days after presentation, the patient reported no complaints, and no evidence of meningoencephalitis was observed. The patient was warned not to fly before a definite diagnostic work up and sealing procedure for the CSF leak site was performed, and the patient was then discharged.
DISCUSSION
The Second World War led to tremendous advances in the technologies related to airplanes and enabled many people to travel by air. Although modern commercial aircrafts provide safe and comfortable travel for most healthy people, the in-flight environment consisting of a lowered barometric pressure, ambient oxygen partial pressure, and low humidity1) could expose a high risk patient (such as the patient discussed here) to danger.
International jet airliners fly at an altitude of 9750 to 11580 meters (32000 to 38000 feet), and domestic airlines fly at 8530 to 8840 meters (28000 to 29000 feet).
Modern jet aircrafts are not pressurized to a sea level equivalent pressure (760 mm Hg).
During flight, the cabin is pressurized to maintain the pressure equivalent to the altitude of 1520 to 2440 meters (5000 to 8000 feet)1). In other words, the cabin pressure is maintained within 536 to 611 mm Hg. Gas in the cabin has been shown to expand its volume by 25-30% during flights3).
Neurosurgical, plastic, and otolaryngologic procedures, especially a craniotomy or skull base surgery, could leave air in the skull and create weak areas where a CSF leak could occur. The traveling patient could potentially encounter two neurosurgical problems : tension pneumocephalus resulting from expansion of the residual air after a craniotomy or a CSF leak through a bony defect made by surgical procedures, resulting in pneumocephalus or pneumomeningoencephalitis.
Until now, there have not been any reported cases of tension pneumocephalus caused by residual air during flight. Donovan et al.7) reported no aggravated cases of neurological deficits and intracranial pressure among twenty-one military casualties with pneumocephalus caused by trauma or a craniotomy during air transport from Iraq to Germany under usual cabin pressure.
Two British studies focused on the medical advice given to post-craniotomy patients regarding air travel and addressed the unstandardized approach of airline companies and insufficient consensus among practicing consultant neurosurgeons2,13).
Several cases of barotrauma-induced pneumocephalus through a weak area have been reported. A cracked tooth5), mastoid air cells10), osteoma of the skull base11), pansinusitis6,9), and a fistulous tract made by cranial4) and spinal8) surgery were suggested as weak areas or causes of weak areas that were susceptible to pressure changes.
In our case, pneumocephalus appeared to occur through the dormant fistulous tract because of the lowered cabin pressure and the synergistic effect of the lumboperitoneal shunt.
The medical guideline recommends waiting at least 7 days to fly after a transcranial procedure or a trauma that introduced gas into the skull without reliable evidence from a plain skull radiograph or CT scan that no air is present. Moreover, a person with a CSF leak from any cause should not fly due to the risk of a backflow of air and microbial contamination1). Although it is difficult to make one guideline to apply to all cases, the concern for possible problems during air travel by patients could lead to consensus among practicing consultant neurosurgeons.
CONCLUSION
Creating guidelines for safe air travel for patients with neurosurgical problems is an important issue to consider because of the frequency with which some patients travel. A consultation with a health care provider addressing the cabin environment and neurosurgical conditions could be helpful for these patients.