INTRODUCTION
Traumatic leptomeningeal cysts (TLMC) are a rare complication of skull fractures, whereby lacerations of the dura mater leads to herniation of the leptomeninges, which in turn fills with cerebrospinal fluid (CSF). This leads to progressive erosion of the skull around the fracture site. Such lesions are especially rare in adults, with only 11 cases detected through a Medline search1,4,7,8). Most incidences of TLMC occur in children <3 years of age; even still, it accounts for only 0.05-0.6% of all pediatric skull fractures3,7,9). Left untreated, TLMC could potentially result in seizures, mental retardation, and increased intracranial pressure. Thus, surgery is usually imperative.
The standard treatment approach involves repair of the dural defect and cranioplasty. Herein, we report the case of a large TLMC located at the vertex of an adult male head, in which the dural repair was performed with fibrinogen-based collagen fleece (TachoCombВ®).
CASE REPORT
A 28-year-old man presented with a growing soft mass on the vertex of his head; it had developed 5 months earlier. Sixteen months prior to this, the patient had been involved in an incident in which he had received a blow to the head. Initially, he had a small subgaleal hematoma but it disappeared by the following day. Patient did not visit hospital for the head trauma; thus, head computed tomography (CT) and X-rays were not performed at that time.
Two years ago, the patient was diagnosed with bipolar disorder, and it was because of this that he underwent a physical examination and EEG for evaluation of his psychological state one month after the incident. At this time, no mass was detected on his scalp. Also, he did not feel the mass on the scalp. It was not until 8 months later that a mass developed, which continued to grow. The patient experienced no associated symptoms, and the mass was not tender to touch. A plain X-ray revealed a round 5Г—5 cm area of lucency in the posterior parietal bone with adjacent skull erosion. Upon enhanced CT examination of the head, a bony defect involving both the inner and outer table of the cranium was observed close to the superior sagittal sinus. A well-defined mass, 5 cm in diameter, was nested within the defect (Fig. 1). There were no enhancing lesions inside the cyst, and the rest of the brain parenchyma was free from notable anomalies. Magnetic resonance imaging (MRI) of the lesion was hypointense on T1-weighted images and hyperintense on T2-weighted images, indicating that a cystic lesion was propagating through the defect and slightly compressing the adjacent brain.
Following this, the patient underwent surgery. A skin flap was created close to the lesion by making an incision down to the galea. The underlying lesion was pulsatile. The galeal layer was then dissected from the cyst, which exposed the cystic membranes. These membranes protruded through the bone defect and contained a clear fluid. The dura around the bone defect was thin and fragile.
Usually, dura is sutured in a watertight manner with artificial dura, such as lyophilic dura. However, due to the close proximity of the defect to the sagittal sinus, we chose instead to place fibrinogen-based collagen fleece (TachoCombВ®) over the dural defect in order to reduce the risk of injuring or perforating the sinus. Six pieces of fibrinogen-based collagen fleece, cut to a size of 1Г—3 cm, were thus placed over the dural defect in a partially overlapping manner. The gluing surface of the fibrinogen-based collagen fleece was attached to the dural defect, exceeding the margins by about 0.5 cm. A wet patty was then applied over the defect and gently compressed. After the patty was removed, any extra seepage of blood was prevented by the application of an additional layer of fibrinogen-based collagen fleece on top of the existing layer (Fig. 2). The outer table of the skull was reconstructed.
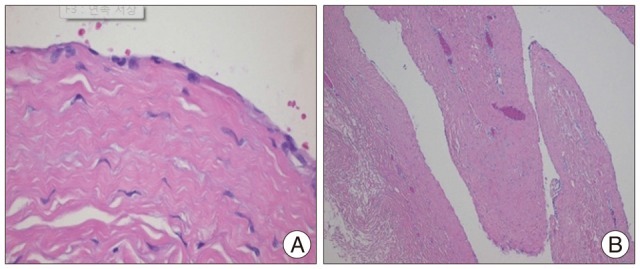
The day after surgery, the patient remained asymptomatic and displayed good cosmetic results. Histologic findings revealed that the cyst was lined by meningothelial cells resting on a layer of supporting fibrous tissue. The walls of the cyst were infiltrated with mild chronic inflammatory cells and displayed vascular congestion. The cyst surface was focally lined with flattened epithelial cells, and the underlying brain tissue had become gliotic. The presence of chronic inflammatory cells and hemosiderin-containing macrophages suggested traumatic etiology (Fig. 3). Thirteen months later, a follow up brain CT scan of the patient revealed no recurrent cystic mass (Fig. 4).
DISCUSSION
An expanding skull fracture is a rare complication of head trauma. It is particularly rare in adults, with 90% of cases reported in infants <3 years of age. Clinically, seizures are the most frequent symptoms of TLMC, reported in over 50% of all patients10). Development of a TLMC can take anything from several weeks to several years to occur after the traumatic incident7). The complicating factor results from a dural tear that accompanies the skull fracture. CSF from the underlying brain tissue, along with the leptomeninges, then herniates through the dural defect, which in turn forms an encapsulated cyst. The continuous pulsatile pressure of the CSF and expansion of the cyst causes resorption of adjacent bone, erodes bone edges and widening of the skull fracture. Theses lesions may progress after s silent period, and may cause a delayed onset of neurological manifestations4,8). Radiological tools for the diagnosis of TLMC include CT and MRI. CT scans are useful for the evaluation of cranial defects and any associated brain lesions. MRI is valuable for distinguishing TLMC from other diseases. The signal intensity of TLMC is equal to that of cerebrospinal fluid (CSF) on both T1-weighted and T2-weighted MRI1). The primary differential diagnoses include osteolytic lesions, such as myeloma, metastasis, epidermoid cyst, and eosinophilic granuloma.
Given the risk of developing seizures, mental retardation, and increased intracranial pressure, surgery is usually imperative. The standard treatment approach for TLMC is minimal extended craniotomy around the defect until normal dura is visualized, followed by watertight duroplasty and cranioplasty; though when primary closure of the dural defect is not possible, a dural graft must be used instead. After the initial introduction of a gold foil to prevent meningocerebral adhesions2), a number of other materials are available for dural repair, including periosteum, fascia lata, fat, muscle, gelatine (GelfoamВ®), freeze-dried dura mater, and methyl methacrylate5).
In this study, due to the close proximity of the dural defect to the sagittal sinus, we opted to use fibrinogen-based collagen fleece (TachoCombВ®), a ready-to-use hemostatic agent consisting of a collagen sheet coated with human fibrinogen, bovine thrombin, and bovine aprotinin. The fibrinogen and thrombin imitate the last steps of the coagulation cascade, whereby upon contact with bleeding wounds or bodily fluids, the coagulation factors dissolve and a link is formed between the collagen carrier and the wound surface. Reddy et al.6) previously used TachoCombRВ® in 288 neurosurgical procedures and concluded that TachoCombВ® is an adequate alternative for dural repair because it is safe, watertight, and efficient, with pleasing surgical properties.
CONCLUSION
Although rare, TLMC can occur in adults. Based on the location of the dural defect, achieving watertight duroplasty is not always possible. We found that fibrinogen-based collagen fleece (TachoCombRВ®) is a valuable and effective alternative approach for dural repair when use of autogenous tissue is not possible and the risk of craniotomy is high.