INTRODUCTION
Exogenous administration of 5-aminolevulinic acid (5-ALA) results in a highly selective fluorescence of the tumor tissue. Its clinical benefits are well established in a wide range of malignancies, especially in high-grade gliomas13). In contrast, its application in meningiomas is only reported infrequently4,7,10). In most cases of meningioma, surgery is the treatment of choice for the prevention of tumor recurrence and postoperative morbidities. Surgical resection using the standard white-light microsurgery is usually uncomplicated. However, rare types of meningioma such as a deep sylvian meningioma reported in this case, can present with unique surgical challenges where 5-ALA-induced fluorescence-guided tumor resection can be of benefit. Believed to arise from the arachnoid cap or meningothelial cells in the Sylvian fissure or the Virchow-Robin space along the middle cerebral artery (MCA) and its branches, deep sylvian meningiomas are usually found deeply buried in the brain parenchyma and are strongly attached to the MCA. To our best knowledge, this is the first experience of 5-ALA in a deep sylvian meningioma reported in the literature.
CASE REPORT
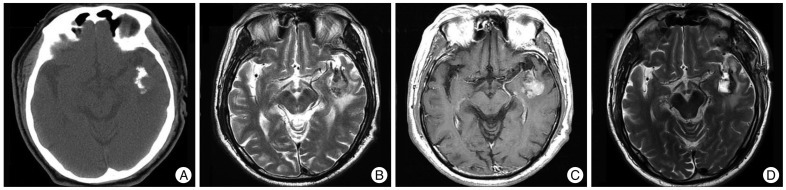
A 69-year-old male was admitted to our hospital upon incidental finding of calcification in the left temporal lobe during a computed tomography scan (Fig. 1A). Magnetic resonance imaging (MRI) revealed a 2.4√ó3.0√ó2.5 cm mass located deeply in the left Sylvian fissure extending into the left temporal lobe. On both T2 and T1-weighted images, it was mainly iso- or hypointense, and enhanced brightly with contrast (Fig. 1B, C). The lesion appeared closely associated with the MCA and was surrounded by moderate edema. Preoperative diagnosis favored an intra-axial tumor, most likely a high-grade oligodendroglioma, which prompted the decision to utilize 5-ALA-induced tumor fluorescence as per standard.
Four hours before the induction of anesthesia, 20 mg/kg of 5-ALA was administered orally. A left fronto-temporal craniotomy was performed, using intraoperative evoked potential monitoring. In order to ensure no interference, the entire operative field was initially assessed for fluorescence with a Leica M720 OH5 microscope (Leica, Wetzlar, Germany) equipped with FL400 Fluorescence Module. After dissecting the Sylvian fissure, a firm mass was exposed and its red fluorescence under the violet-blue excitation light was confirmed (Fig. 2). It was not well demarcated from the surrounding brain parenchyma. The main mass was grossly removed using a cavitron ultrasonic surgical aspirator under white light illumination. Guided by red fluorescence of the remaining tumor tissue, safe excision was achieved, while small areas of neoplasm with calcified portions were preserved due to their strong adherence to the MCA and the sylvian vein. The fluorescence in tumor was of helpful to delineate tumors from vessels which adjoined under same arachnoid membrane and enabled the safe resection without vessel injury.
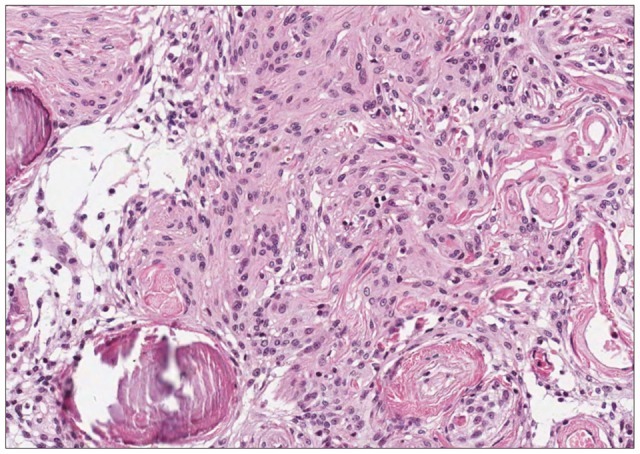
Postoperative MRI (Fig. 1D) demonstrated the aforementioned unresected MCA-adherent neoplastic areas with calcification. Pathological examination of the fluorescent tumor specimen revealed a benign meningioma (WHO grade I) of psammomatous type (Fig. 3). The patient recovered uneventfully without neurological deficits.
DISCUSSION
Deep sylvian meningioma belongs to a rare subtype of meningioma that presents without the "classical" dural attachment. Deep sylvian meningiomas are postulated to originate from the meningothelial or arachnoid cap cells in the pia-arachnoid of the Sylvian fissure and the Virchow-Robin space of the MCA branches. Unlike usual meningiomas, deep sylvian meningiomas occur mostly in young patients and sometimes in the pediatric group3). Adult presentation, such as in our case, is even rarer still. Clinically, the patients most commonly complain of epilepsy or headache. On MRI studies, the lesion is usually iso- or hypointense on both T1 and T2-weighted images, and displays homogenous contrast enhancement. The tumor grows anchored to the MCA and is generally associated with a moderate edema, but rarely with calcifications and intratumoral hemorrhage. However, its radiological appearance is frequently non-specific and a definitive preoperative diagnosis is difficult. Out of the 25 cases of deep sylvian meningiomas that have been reported in the literature2,8,9,12), benign histology is the most common diagnosis (97%)4).
5-ALA is a natural precursor in the heme biosynthesis pathway that, when exogenously administered, results in the accumulation of fluorescent protoporphyrin IX (PpIX) in neoplastic cells with high sensitivity and specificity13). Techniques have evolved that utilizes the 5-ALA-induced tumor fluorescence to assist surgeons in intraoperative diagnosis and differentiation of the neoplastic tissue. Its advantages are well documented in a wide range of malignancies1,5,6,11,14,15). In high-grade glioma where it is most extensively studied, 5-ALA has demonstrated utility as a safe, convenient method that improves the likelihood of complete tumor resection and the progression-free survival, compared to the conventional white-light microsurgery13). The benefit of 5-ALA in meningioma, on the contrary, is more controversial.
Like in other malignancies, 5-ALA-induced fluorescence has been recently reported in meningiomas with high sensitivity (83%) and specificity (100%)4,7,10). Albeit, a different mechanism of accumulation of fluorescent PpIX is proposed in meningiomas, due to their extra-axial origin, in comparison to the high-grade gliomas. Meningioma is a common type of intracranial tumor that is usually benign and slow growing. Maximal tumor elimination by surgery is the treatment of choice. On appearance, the pathology is usually well-circumscribed and a gross-total resection can be achieved with relatively few complications. Hence, the addition of 5-ALA as an adjunct in the surgical treatment of a meningioma may seem initially redundant. However, 5-ALA can still be occasionally useful where meningiomas present with a neurosurgical challenge. Occasionally, a gross total resection of meningiomas can be limited by its complex location and close involvement with neurovascular structures. Tumor micro-invasions to the surrounding structures that were not expected from the preoperative radiology or a lesion that is hidden away from view of the naked eye or the surgical microscope can occur. To this effect, 5-ALA-induced bright fluorescence facilitates the optimal intraoperative tumor visualization, and furthermore, prevents indiscriminate excisions causing injuries to critical normal structures.
In the case presented, the mass was located deep in the Sylvian fissure, and was strongly attached to the nearby MCA and the sylvian vein. Moreover, uncharacteristic of a benign meningioma, the lesion was not well demarcated from the normal brain parenchyma further complicating the surgery. In such situations, aggressive excision with a goal of complete elimination may produce unacceptable postoperative neurological sequelae. With our case, the main tumor mass was removed grossly using the conventional white-light microsurgery. Then, fluorescence guidance was applied to carry out a safe resection. Minimal amounts of the tumor adherent to the vessels - hence, unable to be resected - were preserved.
CONCLUSION
Unlike in malignant gliomas, reports of 5-ALA-induced fluorescence-guided resection in meningiomas are limited. Using the standard white-light microsurgery, a complete excision of meningioma is usually achievable with favorable prognosis. However, less common types of meningiomas can present in complex locations where maximal tumor removal is difficult without causing significant postoperative morbidities. To this effect, the 5-ALA-enabled intraoperative tumor diagnosis may be of assistance. To the best of our knowledge, we report for the first time the experience of 5-ALA in a deep sylvian meningioma suggesting its possible usefulness. Further studies are warranted in order to confirm the benefit of 5-ALA-induced fluorescence in complex meningiomas.