INTRODUCTION
Intracranial dural arteriovenous fistulas (DAVFs) constitute approximately 10 to 15% of all intracranial arteriovenous malformations and are considered to be complex lesions which require careful evaluation in order to determine the most appropriate therapeutic option1,6,11). DAVF with isolated sinus exists in a network of small vessels opening into the wall of a completely thrombosed sinus which does not allow any venous access, either antegrade or retrograde. Consequently, the venous flow goes inversely to the cortical venous system, thus elevating the risk of intracranial hemorrhage3). Despite recent advances in treatment modalities, it is still difficult to treat patients with DAVFs with isolated sinus8). We present our experience with endovascular treatment using the transarterial approach with Onyx (ethyl vinyl alcohol, Micro Therapeutics, Irvine, CA, USA) for DAVF involving an isolated transverse sinus.
CASE REPORT
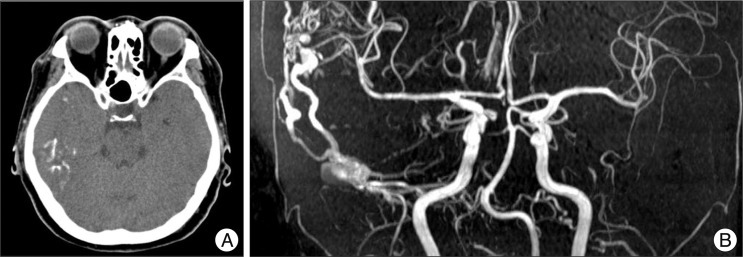
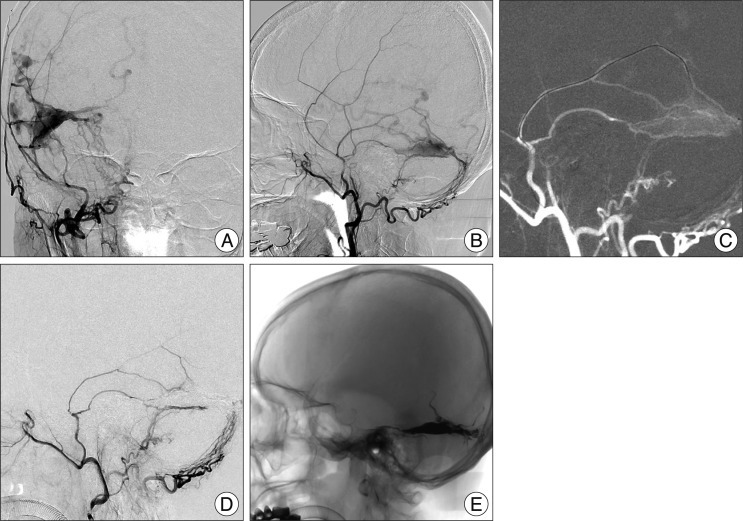
A 69-year-old woman with a two-year history of dizziness and headache was admitted to our hospital after experiencing a generalized tonic clonic seizure. Her clinical examination was normal. She had no history of head trauma. However, six years previously she had undergone a right suboccipital craniectomy and microvascular decompression (MVD) of the facial nerve for a hemifacial spasm. A computed tomography scan obtained at the time of her initial presentation showed curvilinear subcortical calcification and sulcus effacement, predominantly in the right temporal lobe (Fig. 1A). Susceptibility-weighted magnetic resonance imaging (SWI) then demonstrated multiple curvilinear flow voids along the cerebral surface, thus suggesting the presence of a vascular anomaly. Magnetic resonance angiography (MRA) performed to evaluate the possibility of a vascular lesion, revealed a DAVF of the isolated right transverse sinus as well as cortical venous reflux (Fig. 1B). Digital subtraction angiography (DSA) demonstrated a DAVF with an isolated right transverse sinus, supplied by the transosseous branches of the bilateral occipital artery, and the petrosquamous branch of the right middle meningeal artery as well as dural branches from the right vertebral artery. There was retrograde cortical venous reflux (CVR) via leptomeningeal veins from the temporal lobe (Fig. 2A, B). Due to our fear of the risk of hemorrhage or venous infarction associated with CVR, we decided to perform endovascular treatment of the DAVF. Intervention was performed with the patient under general anesthesia. An intravenous bolus of 4000 IU of heparin was administered following placement of a 6-French guiding sheath in the right femoral artery. We initiated the embolization procedures using superselective catheterization of the larger arterial pedicle, which supplied the isolated sinus of the DAVF, in order to achieve the arteriovenous shunt point. A 6-French guiding catheter (Envoy, Cordis Endovascular, Miami Lakes, FL, USA) was placed at the origin of the external carotid artery supplying the meningeal artery chosen for DAVF catheterization. A Marathon microcatheter (ev3 Inc., Plymouth, MN, USA) was then navigated coaxially to access the DAVF under road map (Fig. 2C). The microcatheter lumen was then flushed with dimethyl sulfoxide (DMSO, ev3 Inc., Plymouth, MN, USA). After that, 0.3 mL Onyx-18 was injected within DAVF followed by biplanar simultaneous subtracted fluoroscopy. During the injection of Onyx, special attention was given in order to maintain a steady injection of Onyx, while looking for any reflux of Onyx into the feeding artery along the microcatheter as well as into the cortical vein beyond the isolated sinus. When unwanted flow into a non-targeted areas was observed, the injection was stopped for as long as two minutes. Once the affected sinus was completely packed with Onyx and there was reflux into the feeding artery along the microcatheter, the injection was terminated. The microcatheter was gently pushed back and could then be removed without any complications. Post-embolization angiography showed very slow flow to the right transverse sinus from the occipital artery, and with sequential contrast filling in the right middle meningeal artery, although without evidence of an arteriovenous shunt with early cortical venous drainage (Fig. 2D). The total duration of the Onyx injection was 21 minutes, including eight pauses for reflux. The total procedure time from puncture of the femoral artery to closure of the puncture site was 60 minutes. The patient was discharged five days later and her postoperative course was uneventful. During the next four months, the patient was symptom-free and follow-up magnetic resonance imaging was then scheduled.
DISCUSSION
DAVFs are uncommon intracranial vascular lesions and known to be acquired. Although DAVFs may be found in any dural structures, they occur most frequently in the regions of the transverse, sigmoid, and cavernous sinuses1). Patients with a DAVF may be asymptomatic or may experience symptoms ranging from those which are non-aggressive, (e.g., headache, pulsatile tinnitus) to aggressive symptoms such as hemorrhage, seizures or neurologic deficit. The risk for intracerebral hemorrhage is increased when lesions are in certain locations such as the anterior fossa, and particularly when there is angiographic evidence of CVR. The annual mortality rate for patients with CVR may be as high as 10.4%, whereas the annual risk for hemorrhage or nonhemorrhagic neurologic deficits during follow-up period are 8.1% and 6.9%, respectively, and thus resulting in an annual event rate of 15%15).
DAVF has been reported to develop secondary to sinus thrombosis, trauma or craniotomy5,11,13,16). In cases in which the development is secondary to intracranial surgery, a few authors have reported angiographic identification of DAVF13). Nabors et al.11) reported two cases of postoperative DAVF developing at the surgical site after suboccipital craniectomy, thus suggesting that fistulous development after apposition of the scalp or muscle blood vessels to the dura may be another cause of DAVF development at craniotomy sites. Watanabe et al.16) reported arteriovenous malformations at sites other than craniotomy sites and suspected that indigenous DAVF opened and enlarged under the influence of the change of intracranial pressure after surgery. Considering our patient's previous medical history and the site of the intracranial surgery, we proposed the previous surgery as a possible cause of the DAVF.
Subcortical calcification is a nonspecific imaging presentation. Its frequent causes include Sturge-Weber syndrome, tuberous sclerosis, as well as post-chemoradiotherapy and metabolic disorders secondary to parathyroid or thyroid gland abnormalities. Although the mechanism causing calcification associated with a vascular anomaly has not yet been identified, calcification accompanied by pial arteriovenous malformation is generally considered to be involved in a dystrophic process caused by focal hypoperfusion by steal phenomenon17). In patients with DAVF with CVR, the calcification might be associated with hypoperfusion caused by profuse CVR and the distribution of the calcification may reflect the extent of the venous congestion9). In our case, subcortical calcifications in the right temporal lobe corresponded well with the area of diffuse engorgement of the superficial cortical and deep intramedullary veins identified in the MRA, and DSA.
DAVF with an isolated sinus is a peculiar entity in the sense that venous drainage is done through a thrombosed dural sinus, and it is frequently accompanied by a CVR. This hemodynamic mechanism redirects the blood flow to the cortical venous system, thereby resulting in venous hypertension8). The absence of recanalization of an isolated venous sinus frequently renders an endovascular transvenous approach to be not possible.
The nidus of a DAVF with isolated sinus had two types of arterial irrigation in our case. The fist type is that which originates from a transosseous arterial supply, and which is mainly tortuous and multiple, the transosseous branches of the occipital artery. In this main path for most of the blood flow for the DAVF, it is difficult to perform superselective catheterization. The second type of vascularization for DAVFs is meningeal. Contrary to the transosseous arterial supply, the meningeal artery system penetrates the cranium through its base, thus making the anatomy more navigable and, consequently, more amenable to microcatheterization7). An advantage of using the branches of the meningeal artery is that they are anchored to both the dura and the calvarium. These features, combined with the non-adhesive nature of Onyx, facilitate retrieval of the microcatheter at the end of an Onyx infusion and minimize the risk of arterial rupture4). Several studies have reported high success rates associated with using of the middle meningeal artery (MMA) as the main embolizing arterial pedicle. Nogueira et al.12) obtained complete angiographic cures in 11 of 12 patients when using this method. Cognard et al.2) reported that the fistula was completely obliterated after embolization of one arterial feeder, typically the MMA, in 18 of 24 cases.
A potential advantage of Onyx over n-butyl-cyanoacrylate (n-BCA) is that Onyx embolization may allow for the occlusion of several different vessel feeders from a single pedicle. This therefore avoids the required time and repeated risk of subsequent catheterizations that may be required with n-BCA.
Another consideration regarding the use of Onyx is the prolonged fluoroscopic times. In our case, a single Onyx embolization lasted almost one hour. This drawback must, however, be considered in the context of fewer required catheterizations with the use of Onyx. Theoretically, multiple catheterizations, as required with n-BCA and particulate embolization, also increase the fluoroscopy time. Without a prospective comparison of these agents, we cannot definitely ascertain whether one technique is associated with shorter fluoroscopy times14).
As demonstrated in this case, Onyx offers the possibility of venous sinus occlusion using an arterial side approach which may be quite helpful in cases with previous occlusion of a draining venous structure12).
CONCLUSION
DAVF involving the isolated transverse sinus, and acquired after suboccipital surgery for hemifacial spasm, showed multiple subcortical calcifications associated with venous congestion caused by cortical venous reflux seen on MRA and DSA. We found transarterial Onyx embolization via the middle meningeal artery to be effective for treating DAVF. Owing to the capacity of Onyx to penetrate a shunt and occlude the exit vein, transarterial Onyx embolization can be a good option for curing DAVF with isolated sinus.