Kim, Jin, Jeong, Seo, Ha, and Pyun: Unexpected Detachment of Solitaire Stents during Mechanical Thrombectomy
Abstract
Objective
Unexpected Solitaire stent detachment can occur during mechanical Solitaire thrombectomy. The purpose of this study was to retrospectively evaluate the influencing factors causing unexpected Solitaire stent detachment and the clinical outcomes.
Methods
Between October 2011 to December 2013, 232 cases of mechanical Solitaire thrombectomy for acute ischemic stroke were performed in 3 stroke centers. During this period, we encountered unexpected Solitaire stent detachments during mechanical Solitaire thrombectomies in 9 cases.
Results
Solitaire stents unexpectedly detached in 9 cases (3.9%) during the retrieval of Solitaire stents. The median patient age was 76 years. The occlusion sites of the unexpected stent detachment were the proximal middle cerebral artery (MCA) in 7 cases and the internal carotid artery in 2 cases. The sizes of the stents that unexpectedly detached were 6├Ś30 mm in 7 cases, 5├Ś30 mm in 1 case, and 4├Ś20 mm in 1 case. Four patients had unexpected detachment at the first retrieval, 1 patient at the second, 3 patients at the third, and 1 patient at the fifth. In all of the cases of unexpected detachment at the first retrieval, the stent deployment site was the proximal MCA. After detachment, a proximal marker of the Solitaire stent was observed in 3 patients. However, no marker was visible in the remaining 6 patients.
Conclusion
Unexpected Solitaire stent detachment should be considered in the first instance of stent retrieval for a relatively large-diameter stent, especially in elderly patients with MCA occlusions.
Key Words: Stroke ┬Ę Thrombectomy ┬Ę Stents.
INTRODUCTION
The Solitaire stent (ev3 Inc., Irvine, CA, USA), with its multiple points of contact and engagement with the target thrombus and vessel wall, can distribute outward radial pressure to the segment of vessel that contacts the stent, increasing its potential to capture the thrombus. The use of mechanical Solitaire thrombectomy has been reported to yield favorable outcomes, including positive angiographic results as well as improvement in the incidence of symptomatic intracranial hemorrhage and clinical status 1,2,5,7,8). However, the unexpected detachment of a Solitaire stent can occur during mechanical Solitaire thrombectomy. There are reports of unexpected detachment of solitaire stents 3,6). Furthermore, in vitro investigation of unexpected detachment was observed 4). The purpose of this study was to retrospectively evaluate the influencing factors causing unexpected Solitaire stent detachment and the clinical outcomes.
MATERIALS AND METHODS
Patients
Between October 2011 to December 2013, 232 mechanical Solitaire thrombectomies for acute ischemic stroke were performed in 3 stroke centers. During this period, unexpected detachment of Solitaire stent developed in 9 cases (3.9%) during retrieval of the stent. Local ethics committees approved the use of the patients' retrospective data.
Stroke neurologists performed the neurological assessments using the National Institutes of Health Stroke Scale score. Mechanical Solitaire thrombectomy was generally performed in the patients within 6 hours of symptom onset. The last time the patient appeared normal is shown in Table 1. Large vessel occlusion and the status of the perfusion/diffusion mismatch were confirmed by MR angiography with perfusion, or CT angiography with perfusion, and diffusion imaging. Intravenous recombinant tissue plasminogen activator (dose, 0.9 mg/kg) was administered before the procedure as bridge therapy if the patients fulfilled the inclusion and exclusion criteria for intravenous thrombolysis.
The functional outcome was assessed with the modified Rankin Scale (mRS) score 3 months after the procedure.
Endovascular treatment technique
All patients were treated under local anesthesia with sedative agents. A 6 Fr Envoy guiding catheter (Codman, Raynham, MA, USA) was coaxially introduced into a 6 Fr shuttle catheter (Cook Medical Inc., Bloomington, IN, USA) and placed in the internal carotid artery. The guiding catheters were continuously flushed with normal saline.
In all patients, mechanical thrombectomy was performed using a Solitaire stent. A Prowler select plus (Cordis, Warren, NJ, USA) or an Excelsior XT 27 microcatheter (Stryker, Fremont, CA, USA) was navigated distal to the thrombus over a Synchro 0.014 microwire (Stryker). The distal tip of the microcatheter was positioned approximately 1.5 cm distal to the distal end of the thrombus under confirmation via contrast injection. In our experiences of middle cerebral artery occlusion, small sized or ma-tched sized stent resulted in relative low recanalization rate. Therefore, we selected larger sized stent to prevent migration of the thrombus during stent retrieval. Exceptionally, a small or matched sized stent was selected in cases of severe arteriosclerosis. The Solitaire stent was subsequently advanced to the distal tip of the microcatheter and fully deployed across the thrombotic lesion. The partially re-sheathed Solitaire stent and the delivery microcatheter were removed as a system until the unsheathed Solitaire stent was positioned in the distal tip of the guiding catheter with or without neck compression for flow arrest. Thereafter, the partially re-sheathed Solitaire stent and delivery microcatheter were withdrawn through the guiding catheter. At the same time, continuous aspiration of blood through the guiding catheter was performed in cases of internal carotid artery (ICA) occlusions. Afterward, sufficient blood was aspirated into the syringe through the guiding catheter. A control angiogram was performed to assess recanalization after retrieval of the stent system. The recanalization status was assessed in the final angiogram and classified according to the Thrombolysis in Cerebral Ischemia scale.
RESULTS
Patient demographics, clinical and procedural details are summarized in Table 1. The median patient age was 76 years (range, 57-85 years). Seven patients were female. The median NIHSS score prior to mechanical Solitaire thrombectomy was 17 (range, 7-21). The occlusion sites of the unexpected stent detachment were the proximal MCA in 7 cases and the internal carotid artery in 2 cases. The sizes of the Solitaire stents that detached unexpectedly during stent retrieval were 6├Ś30 mm (7 cases), 5├Ś30 mm (1 case), and 4├Ś20 mm (1 case). In eight patients, the deployment site at the moment of detachment was the acute angle of the MCA that divides the MCA into the M1 and M2 segments ( Fig. 1). In one patient, the site was the ICA bifurcation to the anterior cerebral artery, affecting mainly the A1 segment. In that case, the site was also at an acute angle, and the patient had a carotid T-occlusion. The actual sites of detachment of the Solitaire stents were just inside the acute angle of the MCA that divides the MCA into the M1 and M2 segments in 7 patients, the acute angle of the ICA terminus that includes the ICA and M1 in 1 patient, and the ICA terminus that includes the ICA and A1 in 1 patient. Unexpected detachment occurred in 4 patients at the first retrieval, 1 patient at the second, 3 patients at the third, and 1 patient at the fifth. The patients with unexpected detachment at the first retrieval had the same lesion location (proximal MCA lesion) and stent size (6├Ś30 mm) and were in the same age category (older than 76 years). After detachment, the proximal marker of the solitaire stent was visible in 3 patients. However, no proximal marker was observed in the remaining 6 patients. Immediately after unexpected stent detachment, none of the cases had anterograde blood flow. Several salvage methods were attempted to recanalize the occluded lesions after unexpected stent detachment, including the simple passage of a microcatheter, in-stent balloon angioplasty, double stenting, superficial temporal artery to MCA bypass, craniotomy and stent removal, and intra-arterial chemical thrombolysis with tirofiban. Table 2 outlines the rescue methods employed for each case, as well as clinical and angiographic outcomes. In two of the cases that we assessed, in-stent balloon angioplasty was used. However, MCA rupture occurred in one of those cases, requiring trapping of the MCA with a coil and the superficial temporal artery to MCA bypass procedure ( Fig. 2). In one patient, double stenting was performed with a second, smaller Solitaire stent ( Fig. 3). In an attempt to remove the detached Solitaire stent, stent retrieval with another Solitaire stent was performed in one patient. However, the attempt failed, requiring the performance of a subsequent superficial temporal artery to MCA bypass procedure. The passage of a microcatheter through a detached Solitaire stent combined with tirofiban injection via the microcatheter was performed in two patients. Therefore, the 2 cases achieved partial recanalization. In one patient, only intra-arterial tirofiban injection was performed. However, the case failed to achieve recanalization. Two patients did not undergo a rescue procedure. At the end of treatment, 5 patients had a Throm-bolysis in Cerebral Ischemia score of 0 (two patients underwent a superficial temporal to MCA bypass procedure), 1 patient had a Thrombolysis in Cerebral Ischemia score of 2a, and 3 patients had a Thrombolysis in Cerebral Ischemia score of 2b. The mRS score after 3 months was recorded in 8 patients. One patient had an mRS of 1, one patient had an mRS of 3, four patients had an mRS of 4, and two patients died. Due to loss to clinical follow-up, the mRS after 3 months was not recorded in the final patient. The mRS at discharge was 4.
DISCUSSION
The median age of patients in our study was approximately 10 years higher than that in another study 1,5,7,8). Even if accurate assessment is impossible, this result means that the intracranial vessels of our patients, compared with patients in other studies, may have undergone more atherosclerotic change. Furthermore, a large Solitaire stent may increase the contact area of the vessel wall and stent strut. The friction between the stent and intima of the vessel may increase, which may in turn increase the force required to retrieve the stent. The size of the unexpected detachment of stent which was 6├Ś30 mm in 7 cases may reflect on these. When the stent delivery system cannot tolerate the force, the weakest point of the stent delivery system may break, separating the stent from the rest of the system. In general, stents are supposed to be detached at the detachment zone. However, a review of the angiography results after unexpected detachment of the Solitaire stent revealed cases in which the proximal marker of the Solitaire stent was not visible ( Fig. 1D, 3). Kwon et al. 4) reported that unexpected detachment appeared to be unrelated to the detachment zone. Our results that two thirds of our series showed no proximal marker might support the result of Kwon et al. in vivo. Recently, a new version of the stent retriever has become available that corrects the weak points of the previous version. However, another device-related complications such as vessel dissection or vessel rupture may remain in cases of excessive tensile stren-gth of vessel wall caused by undetached stent. The cases with unexpected detachment during the first retrieval shared some similarities, including stent deployment site (proximal MCA lesions), stent size (6├Ś30 mm), and patient age (>76 years). Because the tortuosity of vessels increases with age, vessel tortuosity and relatively large size stent size may increase the risk of unexpected detachment.
After the stent detached unexpectedly, several methods were attempted as to rescue the stent. Double stenting and passage of a microcatheter with tirofiban injection were relatively successful. Superficial temporal artery to MCA bypass was available as another option of salvage methods. Most of the process of rescue treatments resulted in relative poor prognosis. Therefore, prevention of unexpected detachment is mandatory. Firstly, selection of an appropriately sized stent should be considered in elderly patients with ICA or proximal MCA occlusions. Secondly, sufficient stent re-sheathing of the proximal area before dragging may protect the weakest point of the stent delivery system, increasing the strength of the stent delivery system and decreasing the possibility of unexpected detachment.
This study has limitations, such as being a retrospective study and including a small number of cases. However, our study may be cardinal to evaluate the incidence and influencing factors of unexpected detachment of stents in multi-center trials.
CONCLUSION
In our series, unexpected detachment of a Solitaire stent developed in 9 cases (3.9%). It should be considered in the first instance of stent retrieval for a relatively large-diameter stent, especially in elderly patients with MCA occlusions.
References
1. D├Īvalos A, Pereira VM, Chapot R, Bonaf├® A, Andersson T, Gralla J : Solitaire GroupRetrospective multicenter study of Solitaire FR for revascularization in the treatment of acute ischemic stroke. Stroke 2012, 43 : 2699-2705,   2. Dorn F, Stehle S, Lockau H, Zimmer C, Liebig T : Endovascular treatment of acute intracerebral artery occlusions with the solitaire stent : single-centre experience with 108 recanalization procedures. Cerebrovasc Dis 2012, 34 : 70-77,   3. Kang DH, Park J, Hwang YH, Kim YS : Inadvertent self-detachment of Solitaire AB stent during the mechanical thrombectomy for recanalization of acute ischemic stroke : lessons learned from the removal of stent via surgical embolectomy. J Korean Neurosurg Soc 2013, 53 : 360-363,    5. Mokin M, Dumont TM, Veznedaroglu E, Binning MJ, Liebman KM, Fessler RD 2nd, et al : Solitaire Flow Restoration thrombectomy for acute ischemic stroke : retrospective multicenter analysis of early postmarket experience after FDA approval. Neurosurgery 2013, 73 : 19-25; discussion 25-26,   6. Nayak S, Ladurner G, Killer M : Treatment of acute middle cerebral artery occlusion with a Solitaire AB stent : preliminary experience. Br J Radiol 2010, 83 : 1017-1022,    7. Pereira VM, Gralla J, Davalos A, Bonaf├® A, Casta├▒o C, Chapot R, et al : Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire Flow Restoration in acute ischemic stroke. Stroke 2013, 44 : 2802-2807,    8. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al : Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT) a randomised, parallel-group, non-inferiority trial. Lancet 2012, 380 : 1241-1249,  
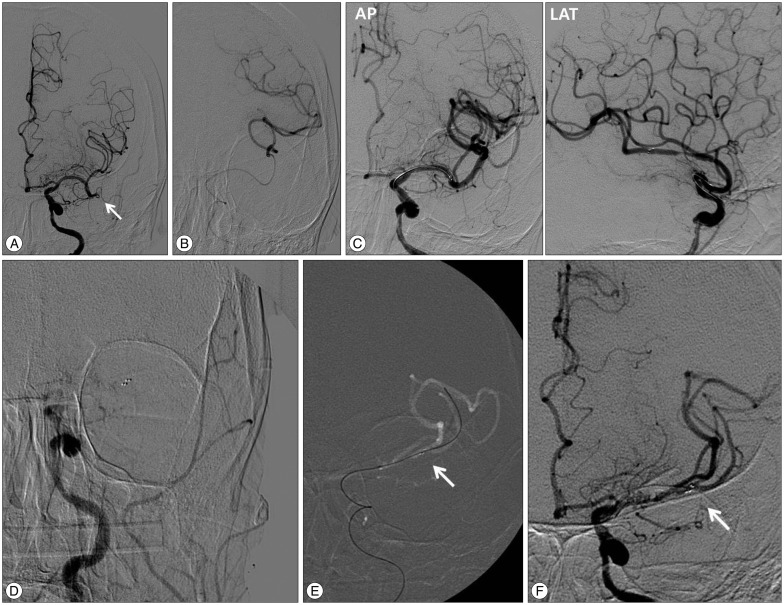
Fig.┬Ā1
A : In patient No. 4, after mechanical Solitaire thrombectomy of a primary lesion (internal carotid artery, cavernous segment), the thrombus migrated to the distal lesion. Left internal cerebral artery angiography reveals occlusion of the inferior branch after the bifurcation of the MCA at the M2 segment (arrow). B : After navigation of the microcatheter via the occluded vessel, selective angiography is performed. C : The anteroposterior (AP) and lateral (LAT) views of left internal carotid artery angiography after the deployment of a Solitaire stent (size : 6├Ś30 mm) reveals partial reopening of the vessel with the stent in situ. D : After unexpected detachment, there is no anterograde blood flow. Furthermore, the proximal marker of the Solitaire stent is not visible. Finally, the Solitaire obviously moved to the internal carotid artery. It appears that the Solitaire is partially retrieved. E : After navigation of the microcatheter with a microwire beyond the thrombus on a map, anterograde flow is restored again. The Solitaire obviously moved to the distal middle cerebral artery. The arrow indicates the distal marker. F : Tirofiban (1.0 mg) injection via a microcatheter is performed. The acute angle of the MCA is changed to an obtuse angle (arrow). Furthermore, compare with immediately after unexpected detachment, the Solitaire stent moved to the distal area. MCA : middle cerebral artery. 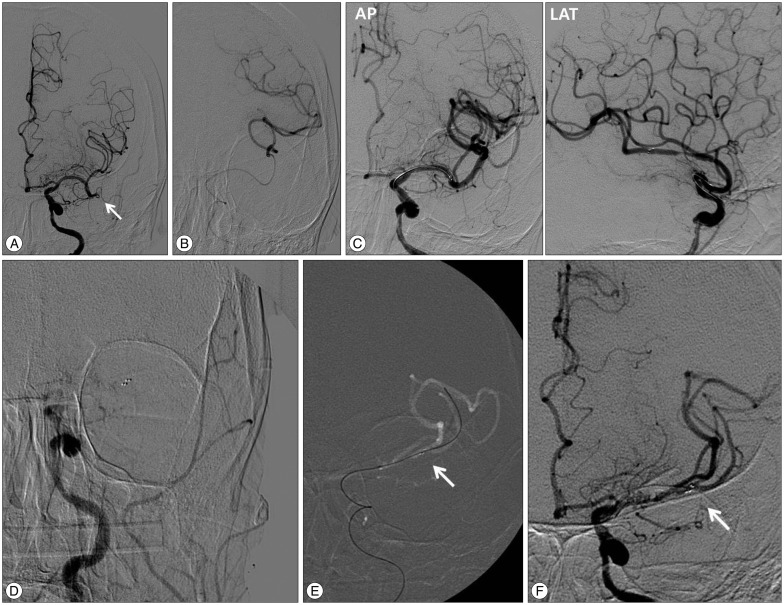
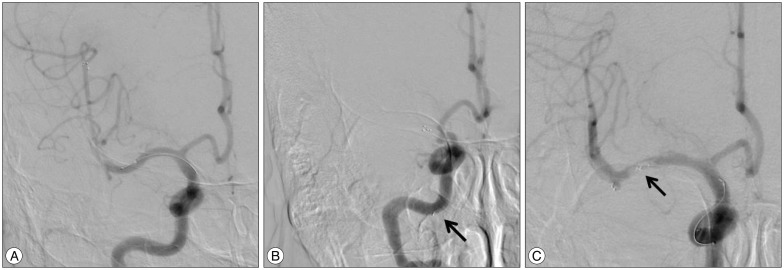
Fig.┬Ā2
A : After unexpected detachment, in stent balloon angioplasty with a double-lumen balloon catheter is performed (patient No. 1). B : Because of MCA rupture during balloon angioplasty, contrast leakage is observed. C : Internal trapping with a coil via the double-lumen balloon catheter is performed. 
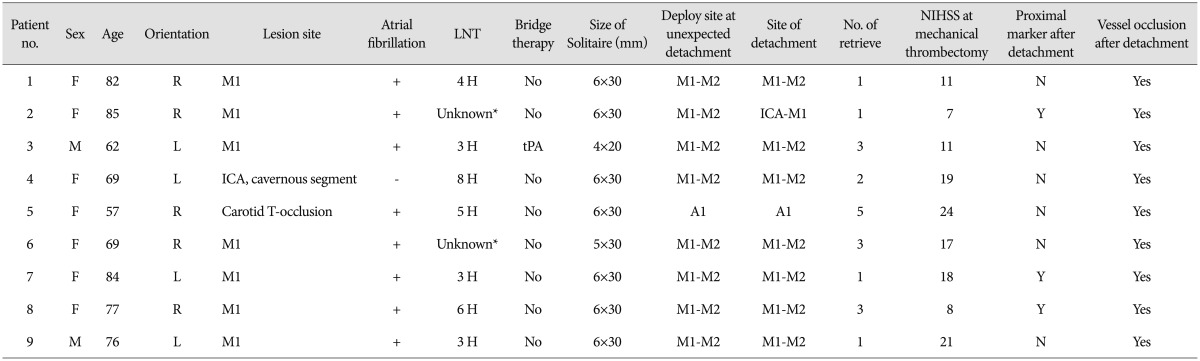
Fig.┬Ā3
A : An anteroposterior view of the right internal carotid artery angiography after deployment of a Solitaire stent (size 6├Ś30 mm) in patient No. 2 reveals partial reopening of the MCA flow with the stent in situ. B : After unexpected detachment, there is no anterograde blood flow. The solitaire obviously moved to the internal carotid artery. In this case, the proximal marker of the Solitaire stent is visible (arrow). C : Double stenting is performed with a second, smaller Solitaire stent (4├Ś20 mm). Compare with immediately after unexpected detachment, the Solitaire stent moved to the distal area. The thrombus that was caught by the distal marker of the first Solitaire stent is visible (arrow). Anterograde flow is restored again. 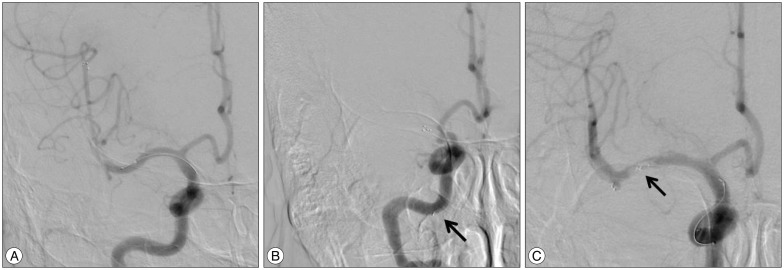
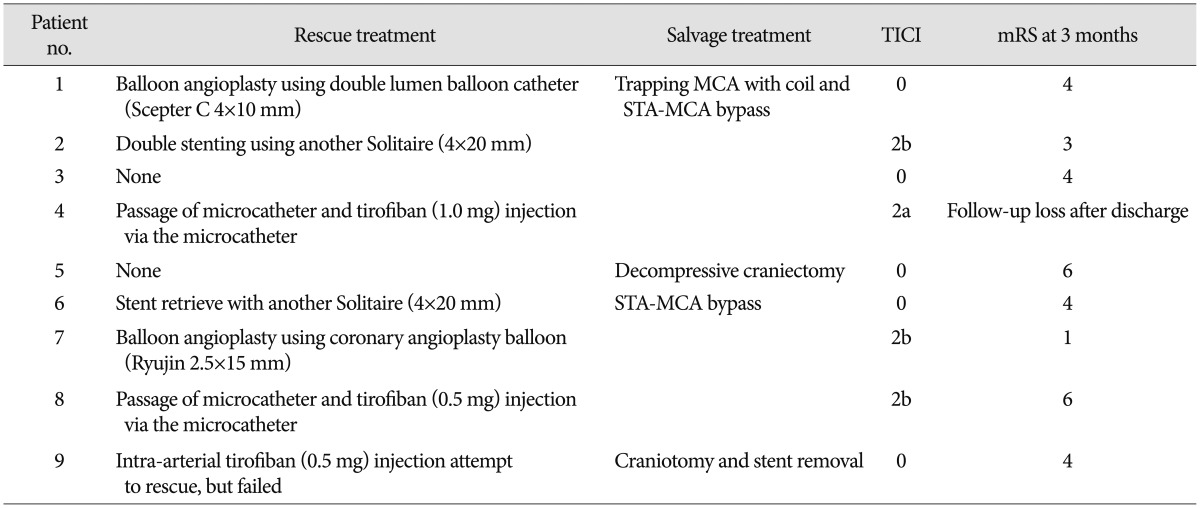
Table┬Ā1
The angiographic and clinical presentation of the patients who had unexpected detachment of a Solitaire stent 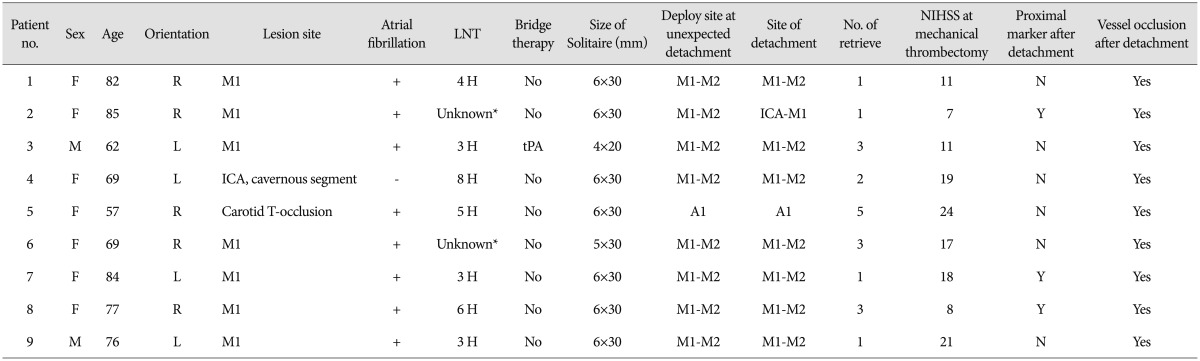
Table┬Ā2
Rescue treatment and angiographic and clinical outcome of the patients with unexpected detachment of a solitaire stent 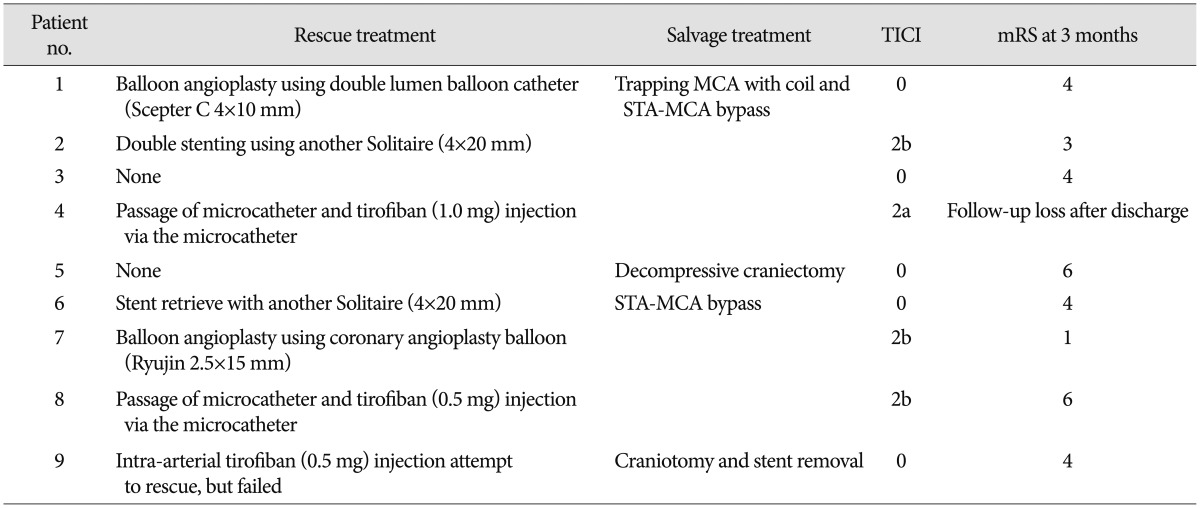
|
|