INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is the gold standard for the surgical treatment of cervical disc disease. Many modifications of this technique have been reported since its original description by Smith and Robinson1,5,7,9,10,12,17,19,21-24).
In the early days of ACDF, autologous bone grafts from the iliac crest were used, however, they caused various donor site morbidities including pain, numbness and infection2,13,19,21). To overcome these disadvantages, allobone or bone substitutes like demineralized bone matrix have been used, but those include the risk of pathogen transmission as well as relatively lower fusion rate and high additional costs10,17,18,21).
A few surgeons have used the implantation of an empty cage during the ACDF, however, they have not reached a general agreement due to the suspicion of low bone fusion rate17,18).
Using a plate system has several advantages including increased stability, prevention of graft extrusion and increased bone fusion rate, but it has also high additional costs and the risk of hardware failure10,20).
Recently, ACDF using a stand-alone cage packed with local autobone graft has been used with favorable results5,9,13,16,25). According to Shad et al.21), ACDF with a stand-alone cage packed with local bone graft has good clinical and radiological outcomes without iliac donor site morbidity and high additional costs. However, nonunion and subsidence into the endplates have been reported as complications of this procedure5,11,12,23). A previous study of stand-alone cage packed with bone graft by Bartels et al.5) reported that subsidence occurred in 29.2% and nonunion occurred in 4.3%. In a similar study of stand-alone cage packed with cancellous iliac bone graft by Yang et al.25), they reported that subsidence and nonuinion occurred in 25.5%, 14.9%. However, according to their reports, in spite of the risk of subsidence and nonunion, clinical outcomes were relatively good in the subsidence and nonunion groups.
In our institute, autologous iliac bone graft and allobone graft are not used for ACDF in non-traumatic single level degenerative cervical diseases. Instead, we perform ACDF using a stand-alone cage packed with local autobone graft from the lower anterior lip of the upper vertebral body and an osteophyte at the anterior and posterior vertebral body.
The purposes of the present study were to evaluate the clinical and radiological outcome including bone fusion and subsidence which occur after ACDF using a stand-alone cage packed with local autologous bone graft.
MATERIALS AND METHODS
Patient demographics
From July 2009 to December 2011, thirty-one consecutive patients who underwent single level ACDF for degenerative cervical disc disease without the anterior plating system or allobone graft were included in this study. We used a stand-alone cage packed with local autobone graft instead of autologous iliac bone graft or allograft.
Exclusion criteria were multilevel or traumatic cervical disc disease, using the plate system.
The mean age of these patients at the time of operation was 51.4 years (range 30-74). There were 15 males and 16 females with a mean follow up period 12 months (8-16 months). Twenty one patients had soft disc herniation, and 10 patients had cervical spondylosis. C5-6 was most the frequently treated level (C3-4 : 4 cases, C4-5 : 7 cases, C5-6 : 17 cases, C6-7 : 3 cases).
Surgical technique
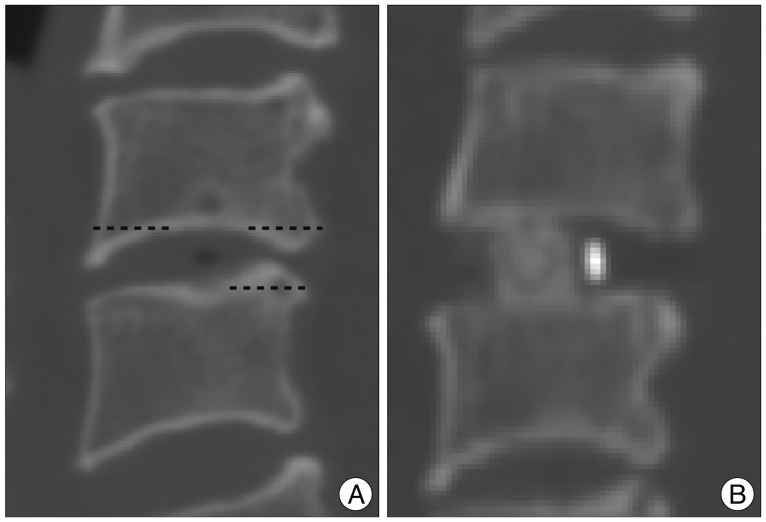
We used the standard technique described by Smith and Robinson1,5,7,9,10,12,17,19,21-24). After soft tissue dissection and annular incision, total discectomy was done. The lower anterior lip of the upper vertebral body and osteophytes at the anterior and posterior aspect of the vertebral bodies were carefully removed parallel to the endplate using a Kerrison punch (Fig. 1A). During the whole operative procedure, we did not drill out the vertebral bodies and osteophytes.
After a thorough and careful preparation of both endplates so not as to damage the bony endplate, a PEEK cage (Cervios cages®, Synthes, Oberdorf, Germany) packed with these local autobone chips was implanted in the disc space under the fluoroscopic guide (Fig. 1B). Anterior cervical plates were not used in all patients.
Outcome measurement
Medical charts, imaging studies, and outcomes of patients were analyzed. All patients were preoperatively assessed using their initial anterior and lateral conventional radiographs, 3-dimensional computed tomographic (CT) scans, and magnetic resonance images. Follow-up studies included cervical spine radiography (in AP-lateral views) at 6 weeks and at 3, 6, and 12 months after surgery, and 3-dimensional CT scans of the cervical spine at immediate postoperative and 6 or 12 months after surgery.
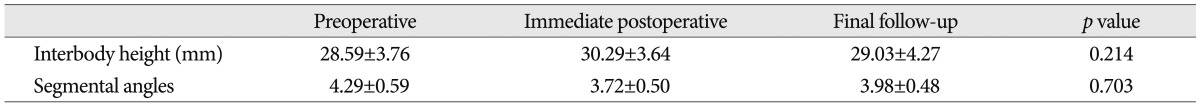
Interbody height (IBH) was measured by CT as the distance between the middle points of the upper end plate of the superior vertebral body and the lower end plate of the inferior vertebral body (Fig. 2A). Segmental angle (SA) was defined as the angle between the upper end plate of the superior vertebral body and the lower end plate of the inferior vertebral body, as measured by Cobb's method (Fig. 2B).
Subsidence was defined as a decrease of the interbody height more than 2 mm in immediate post operative CT and last follow up CT. Solid bone fusion was defined as the establishment of a solid bone bridge between fusion segments on the last follow up CT scans.
Clinical assessment involved the use of a Visual Analogue Scale (VAS) score, neck disability index (NDI), and modified Odom's criteria. Modified Odom's criteria was classified by 4 grades; excellent, good, fair, and poor. Excellent is defined as complete relief of symptoms, good as intermittent discomfort, but no interference with daily activities, fair as subjective improvement but impaired physical activity, poor as no improvement at all, and worse as actual worsening of the symptoms4,5).
Statistical analysis
The statistical analysis was performed using SPSS version 17 for Windows (SPSS Inc., Chicago, IL, USA). All data were reported as mean┬▒standard deviations. Significant differences were determined using the paired t-test between immediate postoperative values and last follow up values of interbody height and segmental angle. Two-sided probability testing was used, and a probability value Ōēż0.05 was considered statistically significant.
RESULTS
Radiological outcomes
Table 1 summarizes the radiological outcomes including IBH and SA. The mean IBH of immediately after surgery was 30.29┬▒3.64; this value decreased to 29.03┬▒4.27 mm at last follow up. The mean loss of IBH between immediately after surgery and last follow up was a difference of 1.26┬▒0.44 mm, which was statistically not significant (p=0.214). The mean SA after surgery was 3.72┬▒0.50, this value changed to 3.98┬▒0.48 degrees at last follow-up.
Cage subsidence of greater than 2 mm occurred in 7 of 31 patients (22.6%). Subsidence between 2 and 3 mm developed in 3 patients, and subsidence over 4 mm developed in 4 patients.
On the last follow up CT scans, solid bone fusion was present in 28 patients (90.3%), and nonunion occurred in 3 patients (9.7%). Twenty-four patients without subsidence showed complete fusion. Of 7 patients with subsidence, 3 patients had nonunion (42.9%) while the other 4 patients had fusion (57.1%). In the subsidence group, 3 patients with a mild subsidence of 2-3 mm were all fused, but patients with a subsidence of over 4 mm had nonunion except in only one patient (75%) (Table 2).
Clinical outcomes
All thirty-one patients showed improvement in their symptoms after surgery. The mean pre-operative VAS was 6.63┬▒1.71 and follow up was 1.80┬▒1.10. Pre-operative NDI was 20.61┬▒9.75 and follow up was 9.20┬▒5.10. Decreases in VAS and NDI were statistically significant compared with pre-operative data (p=0.000).
According to modified Odom's criteria, seventeen (54.8%) patients had an excellent outcome and fourteen (45.2%) patients had a good outcome. Four patients in the subsidence group had an excellent outcome, and other three patients had a good outcome. Despite the occurrence of subsidence or nonunion, clinical outcomes of all patients with subsidence Ōēź2 mm or nonunion were excellent or good, thus additional surgery was not performed.
DISCUSSION
Traditionally, autologous iliac bone graft has been used to fill the disc space during ACDF2,6,7,11,15,22,24,25). In spite of a high solid bone fusion rate and good clinical outcome, implantation of autologous iliac bone graft comes with the consequences of donor site morbidities including pain, numbness, and infection2,13,19,21).
As a result, the use of a stand-alone cage has become popular, and many reports have described its effectiveness such as stability, restoration of the disc height, and facilitation bone fusion. However, nonunion and subsidence have been reported as complications of ACDF using stand-alone cages3,5,8,9,13,25). There are various types of cages, and various materials are used for filling the cages, although controversy exists regarding the type of filling material in the cage1,10,13,14,20,21). Many surgeons use cancellous iliac bone graft to fill the cages. Vavruch et al.24) studied the fusion rate between autologous iliac bone graft and a cage packed with cancellous bone graft from the iliac crest, and they showed a lower fusion rate in the cage group (62% compared with 86% in the iliac bone graft group)19). Although they insisted cancellous bone graft from the iliac crest due to its lower invasiveness, it still brings about the complications of donor site pain and morbidity compared with iliac bone graft. Some authors use cages without any filling material. However, the use of cages without any filling material is still questionable. Ioannis et al. performed anterior cervical discectomy and implantation of empty PEEK cages and showed a lower fusion rate of 71.7% (43 of 60 cases)17,18).
Payer et al.17) reported the implantation of an empty carbon fiber cage after single level ACDF; the bone fusion rate was 98% (24 of 25), and significant subsidence over 2 mm occurred in 20% (4 of 20)18). However, since their study evaluated subsidence and fusion by simple X-ray, fusion rates might be overestimated.
Other authors have reported using allobone or bone substitute as filling material. Using the allobone has a risk of pathogen transmission and using the bone substitute would need additional costs9,10).
Bartels et al.4,5) reported subsidence and nonunion after implantation of stand-alone cages packed with autologous cancellous iliac crest, in that study subsidence and nonunion occurred in 29.2% and 4.3%.
In our study, local autobone graft from the lower anterior lip of the upper vertebral body and osteophytes at the anterior and posterior aspects of the vertebral bodies were used to fill the PEEK cage. The volume of local bone from the anterior lip is not enough to fill the cage, but enough volume could be collected from the osteophyte at the posterior part of the vertebral body with a Kerrison punch. Min et al.14) compared osteogenic differentiation potentials of bone marrow stem cells obtained from the vertebral body and iliac crest. Their study showed the bone marrow stem cells from the vertebral body had osteogenic differentiation potential similar to those from the iliac crest. Although the biochemical and molecular characteristics of osteophytes may not be comparable with those of stem cells, the vertebral body would be an appropriate graft material to fill the cage. Shad et al.21) reported the use of local bone dust created during drilling of osteophytes to fill the cages, and assessed the clinical and radiological outcomes. In their study, clinical outcomes were relatively good, but solid bone fusion occurred in 17 of 22 patients (77.2%). The bone fusion rate was lower than our study, we thought this result could be associated with the quality of bone dust. They used bone dust collected by the suction trap method after drilling, which means that the volume of the bone material might not have been enough. We collected bone chips using a Kerrison punch from not only the anterior lip but also from the posterior body without drilling. However, a relatively enough volume of bone chips could be collected.
In the study by Pitzen et al.20) (91.3% fusion rate), using local autobone grafts had good radiological outcomes. They used the anterior plate system; however, using the anterior plate system will need additional costs. Although we did not use the anterior plate system, a similar bone fusion rate (90.3%) was achieved compared with their study, along with good clinical outcomes.
There are several risk factors of subsidence and nonunion that are frequently mentioned in other studies5,9,12,23,25). Wrong surgical techniques such as overdistraction, damage of endplate, and insufficient preparation of endplate are some examples. Likewise, in the present study, endplate damages occurred during the operation in three of seven subsidence cases. Adequate preparation of the both endplates so as not to damage the bony cartilage would be an important factor to decrease subsidence after ACDF with a stand-alone cage.
Bartels et al.4,5) reported that the incidence of subsidence was statistically higher at C6-7 levels. They thought that the orientation of C6-7 causes higher stress shielding and it would be possible reason. However, Two cases of subsidence occurred in 7 subsided patients in our study, so according to our opinion, fused level was not significantly associated with subsidence.
Except patients with endplate damage, most patients in the subsidence group were over 60 years old. Although we could not evaluate bone mineral density in all patients, osteoporotic change in the vertebral body can be thought as a risk factor of subsidence. Therefore, surgeons should check the presence of osteoporosis before surgery to predict the risk of subsidence.
In our study, of seven patients with subsidence, three patients had nonunion while the other four patients had fusion but all patients without subsidence showed solid bone fusion. Therefore, subsidence is thought to be a risk factor of nonunion. Despite the occurrence of subsidence and nonunion, all patients showed resolution of neck and arm pain.
CONCLUSION
Although the use of a stand-alone cage packed with local autobone graft has a risk of subsidence, clinical outcomes and fusion rates are good enough compared with other methods.
With deliberate selection of patients and adequate preparation of the endplate, stand-alone cages packed with local autograft will be used as good alternatives to decrease donor site morbidity and additional costs required by other methods.