Woo, Yang, Lee, Lee, Kim, and Hong: Continuous Low-Dose Temozolomide Chemotherapy and Microvessel Density in Recurrent Glioblastoma
Abstract
Objective
The purpose of this study was to evaluate the clinical efficacy of continuous low-dose temozolomide (TMZ) chemotherapy for recurrent and TMZ-refractory glioblastoma multiforme (GBM) and to study the relationship between its efficacy and microvessel density within the tumor.
Methods
Thirty patients who had recurrent GBM following Stupp's regimen received TMZ daily at 50 mg/m2/day until tumor progression between 2007 and 2013. The median duration of continuous low-dose TMZ administration was 8 weeks (range, 2-64).
Results
The median progression-free survival (PFS) of continuous low-dose TMZ therapy was 2 months (range, 0.5-16). At 6 months, PFS was 20%. The median overall survival (OS) from the start of this therapy to death was 6 months (95% CI : 5.1-6.9). Microvessel density of recurrent tumor tissues obtained by reoperation of 17 patients was 22.7┬▒24.1/mm2 (mean┬▒standard deviation), and this was lower than that of the initial tumor (61.4┬▒32.7/mm2) (p-value=0.001). It suggests that standard TMZ-chemoradiotherapy reduces the microvessel density within GBM and that recurrences develop in tumor cells with low metabolic burden. The efficacy of continuous low-dose TMZ could not be expected in recurrent GBM cells in poor angiogenic environments.
Conclusion
The efficacy of continuous low-dose TMZ chemotherapy is marginal. This study suggests the need to develop further treatment strategies for recurrent and TMZ-refractory GBM.
Key Words: Glioblastoma ┬Ę Temozolomide ┬Ę Metronomic chemotherapy ┬Ę Microvessel density.
INTRODUCTION
The prognosis of glioblastoma (GBM) patients still remains poor despite advances in surgical techniques, radiotherapy and chemotherapy. The median overall survival is expected to be only 14.6 months after maximum safe resection and irradiation with concurrent temozolomide (TMZ) and adjuvant TMZ chemotherapy. In spite of multimodal therapies, most patients suffer recurrence and die within forty weeks 13,22). However, there is no consensus on the treatment for recurrent and TMZ-refractory GBM. Bevacizumab, a humanized monoclonal antibody against vascular endothelial growth factor (VEGF)-A, has been shown to have significant biological activity in patients with recurrent GBM and has been under investigation with other target agents 12). Nitrosourea-based chemotherapy is associated with the risk of severe hematological toxicity 32). Rechallenge with alternative dosing TMZ for recurrent GBM is recommended, even if the patient has a history of standard TMZ chemotherapy 6,30). Continuous therapy with metronomic regimens was reported to inhibit tumor angiogenesis through the suppression of tumor endothelium regeneration and MGMT depletion of the tumor endothelium 9,1011,25). On such a theoretical basis, dose-dense TMZ chemotherapy has been investigated for the treatment of recurrent or TMZ-refractory GBM despite ongoing debates on their clinical efficacy 23,29). Considering the grim prognosis of recurrent GBM and the cost effectiveness of chemotherapy, it is important to clarify the clinical efficacy of continuous low-dose TMZ chemotherapy and to incorporate biomarkers to predict the response. In the present study, we focused on the pathologic features and clinical courses of recurrent and TMZ-refractory GBM treated with continuous low-dose TMZ (50 mg/m 2, daily) until tumor progression. Microvessel density is considered a surrogate marker of neovascularization by detecting endothelial cells of the tumor micorvasculature 3,24). Several studies have indicated that microvessel density is an important prognostic factor in various malignancies 4,1719). We analyzed prognostic value of the microvessel density of GBM cells obtained by surgical interventions.
MATERIALS AND METHODS
Patient characteristics
From January 2007 to May 2013, 30 patients diagnosed with recurrent and TMZ-refractory GBM were given a dose of 50 mg/m2 TMZ daily until disease progression or the decision to discontinue by the care giver at our institution The patients had previously been treated with concurrent chemoradiotherapy (CCRT) with adjuvant TMZ following the initial diagnosis of GBM. The first surgery achieved total resection, subtotal resection and biopsy in 16, 10, and 4 patients, respectively. The median Karnofsky performance status (KPS) scale at the time of first diagnosis was 90 (range, 70-100).
Recurrence was determined by pathological examination in 17 patients and radiological findings according to Macdonald's criteria 15) in 13 patients. TMZ was administered orally everyday at 50 mg/m 2/day until neurological or radiological deterioration developed. The patients were asked to fast for four hours prior to and two hours after administration. Full blood examination was performed every 4 weeks. Clinical characteristics are summarized in Table 1. Toxicity grading was evaluated according to the National Cancer Institute Toxicity Criteria (v4.0).
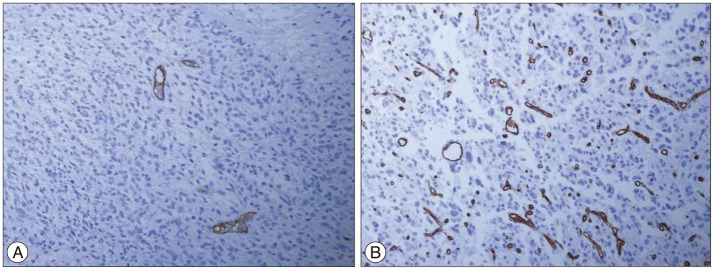
Microvessel density
Resected specimens were fixed in 10% formalin and embedded in paraffin. Thin sections (4 ┬Ąm) were deparaffinized twice using xylene and rehydrated in ethanol. The sections were placed in 0.01 mol/L of trisodium citrated dehydrate buffer (pH 6.0), and then treated in a microwave oven for 10 min at 500 W. For CD34 staining, the tissue sections were digested with 0.2% trypsin in 0.01 mol/L phosphate-buffered saline (PBS) for 20 min at 37Ōäā. Next, the tissues were immersed in 3% H2O2 with distilled water for 10 min to inactivate endogenous peroxidases. After blocking non-specific binding by normal goat serum, the sections were incubated overnight at 4Ōäā with mouse anti-monoclonal CD34 antibody (QBEnd10 clone, 1 : 100, Dako, Glostrup, Denmark) as the primary antibody. Counterstaining was performed for 1 min with Mayer's hematoxylin. Images were acquired using an Olympus BX41 microscope (Olympus, Tokyo, Japan) with a Camedia digital camera. The immunostained slides were examined under light microscopy by two of the authors who were blinded to the patients' clinical histories. Tumor microvessel density was determined by calculating the mean number of any endothelial cells stained with CD34 in three areas of highest vascularization in each slide under ├Ś200 magnification.
Statistical analysis
Progression-free survival time (PFS) was estimated from the start of continuous low-dose TMZ administration to tumor progression or drop-out from the study. Overall survival (OS) was from the start of continuous low-dose TMZ to the date of death, irrespective of its cause. PFS and OS were assessed by the product-limit method of Kaplan-Meier for all patients, and it was performed by using the SPSS software package (version 18.0, SPSS Inc., Chicago, IL, USA). The local ethics committee gave approval for this work.
RESULTS
Clinical outcomes
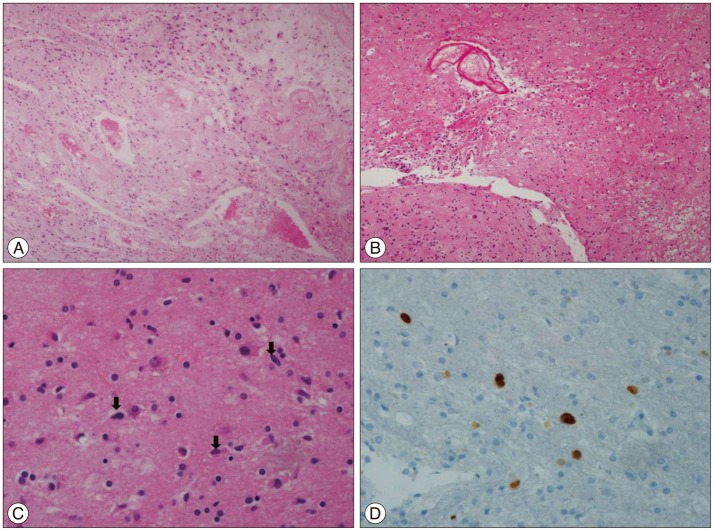
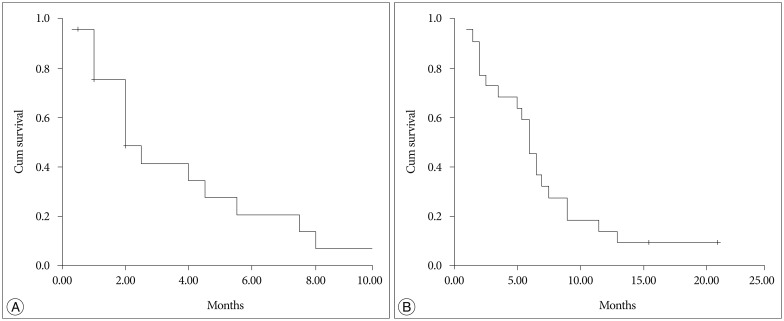
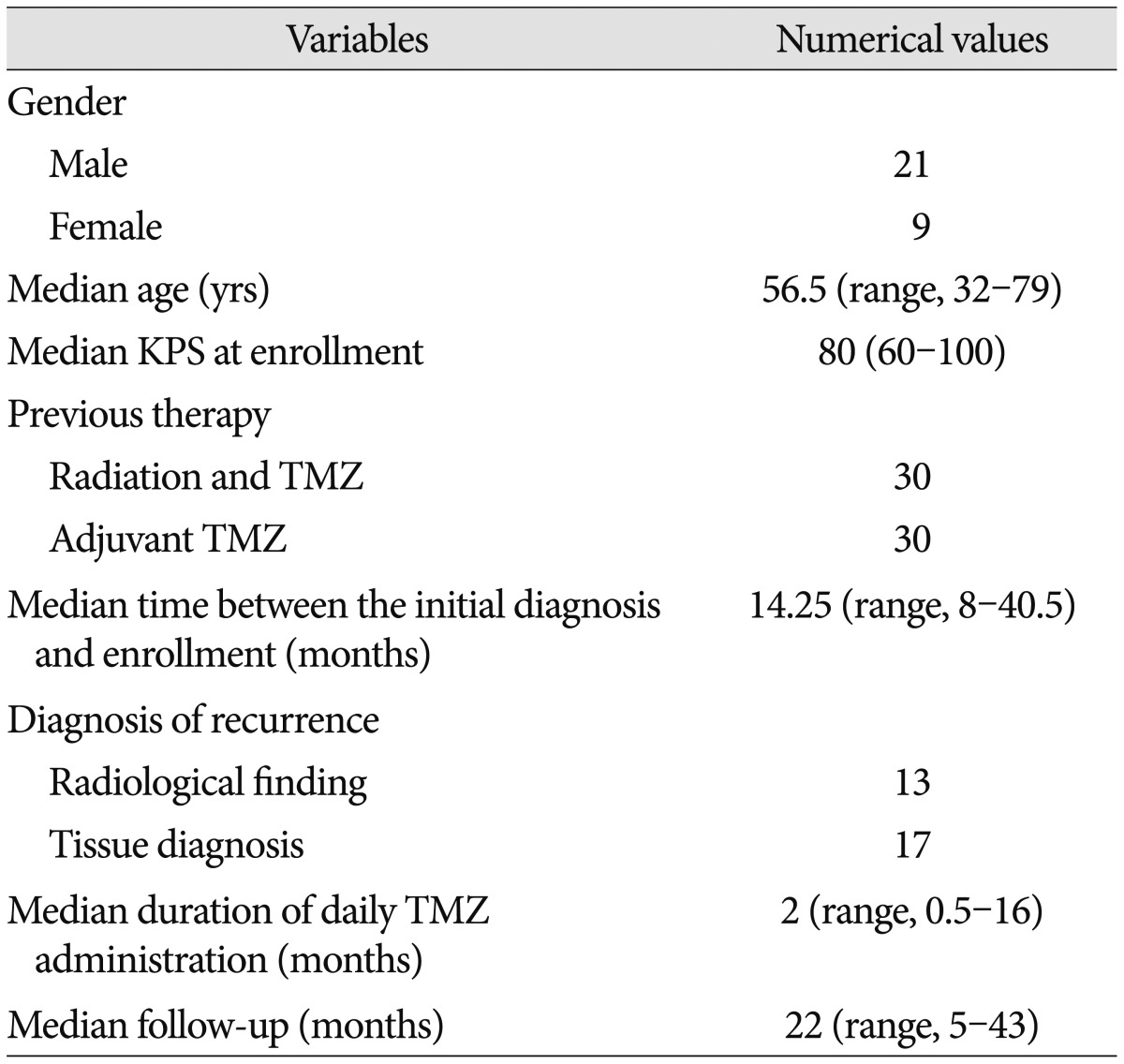
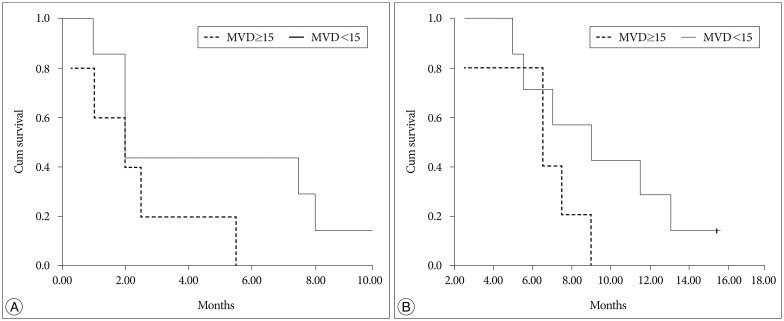
The patient population included 21 males and 9 females with a median age of 56.5 years (range, 32-79). The median KPS at enrollment was 80 (range, 60-100). All patients were previously treated with CCRT and adjuvant TMZ chemotherapy only. Seventeen out of 30 patients underwent reoperation, and among them, grossly total resection and subtotal resection were achieved in 4 and 13 patients, respectively. Reoperation was used for confirmation of recurrent disease or for debulking to provide symptoms relief. The histological findings showed recurrent GBM in 15 patients and mostly radiation necrosis with viable tumor cells in 2 ( Fig. 1). The median time between the initial GBM diagnosis and low-dose continuous TMZ administration was 14.25 months (range, 8-40.5). The median duration of low-dose continuous TMZ administration was 8 weeks (range, 2-64). The median overall survival (OS) from the initial diagnosis was 22 months [95% confidence interval (CI) : 15.2-28.8]. The median progression-free survival (PFS) of continuous low-dose TMZ therapy was 2 months (95% CI : 1.0-2.9). The 6-months PFS was 20%. The median OS from the start of low-dose, continuous TMZ administration to death was 6 months (95% CI : 5.1-6.9) ( Fig. 2). Toxicity including nausea, vomiting and dizziness was well tolerated. Grade III and IV hematologic toxicity did not occur.
Clinical impication of microvessel density
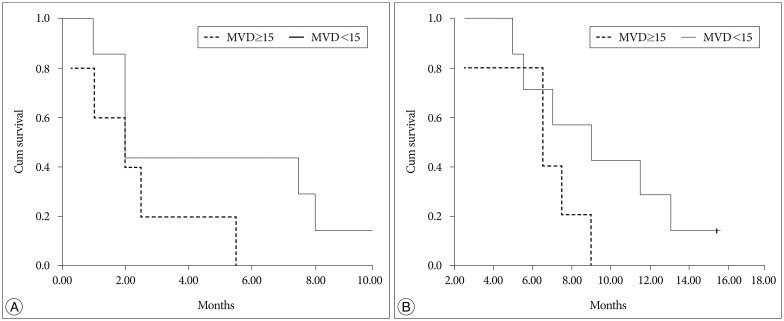
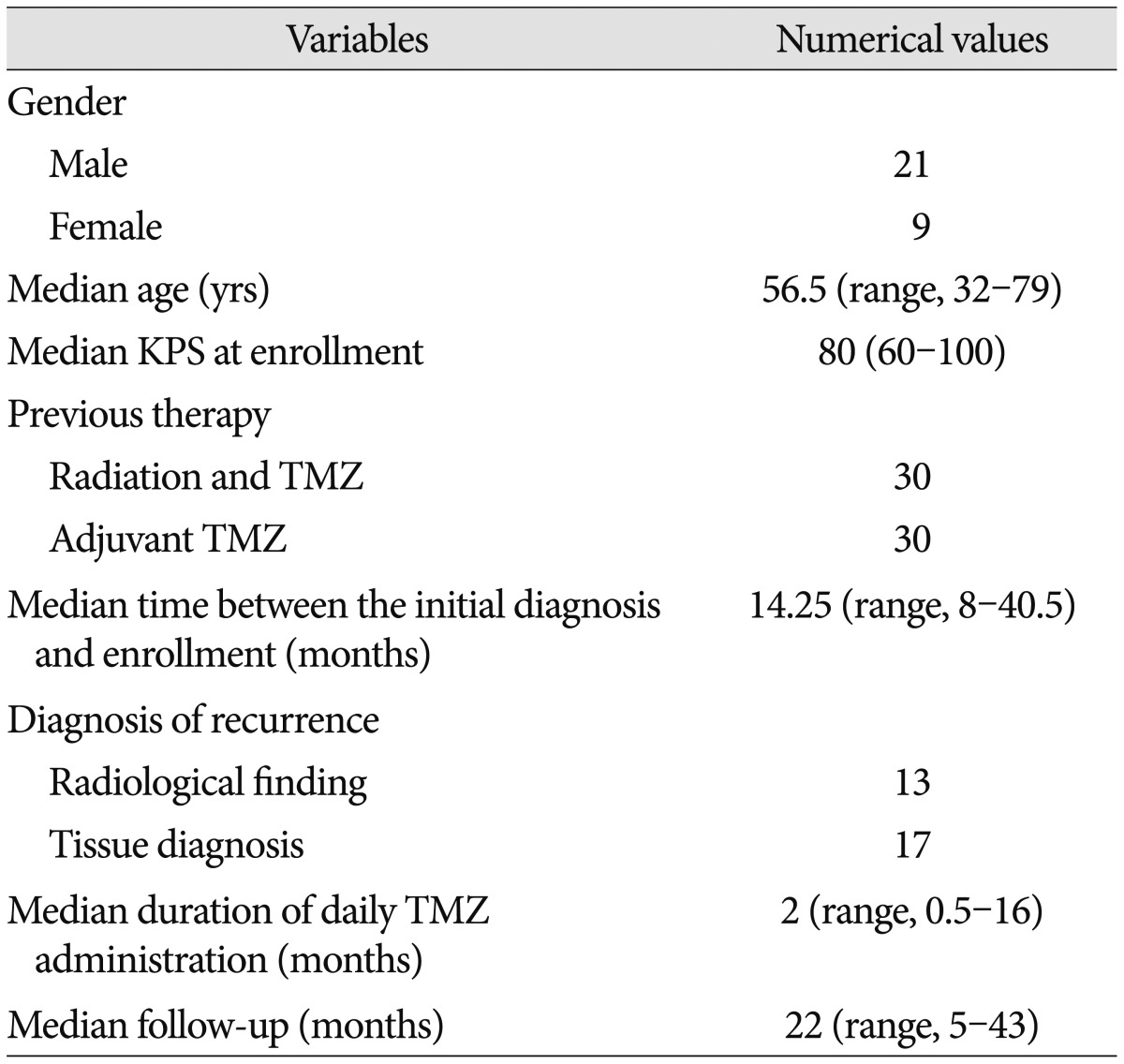
Immunohistochemical staining (IHC) for microvessel density was performed to examine the role as the prognostic factor in the recurrent specimens obtained by surgical interventions ( Fig. 3). The median microvessel density within recurrent tumor area obtained by reoperation was 15/mm 2 (range, 3-97), and this value was applied as a cut-off value. OS and PFS tended to be better in the lower microvessel density group than in the higher density group, but this finding was not statistically significant ( p-value=0.156 and 0.144, respectively) ( Fig. 4). The microvessel density of the first specimen obtained by the initial operation was 61.4┬▒32.7/mm2 (mean┬▒standard deviation). The value was higher than the microvessel density of 22.7┬▒24.1/mm2 in the recurrent specimen (p-value=0.001).
In analyzing 17 patients underwent reoperation, the microvessel density of the first specimen (65.5┬▒11.4/mm2) was higher than that of the recurrent specimen (p-value=0.001). A median microvessel density of 55/mm2 and 15/mm2 was applied as a cut-off value in the initial and recurrent tumor, respectively. The median OS (35 months) of patients with low microvessel density in the initial specimens and low microvessel density in the recurrent specimens tended to be higher than that (22 months) of patients with high microvessel density in the initial specimens and high microvessel density in the recurrent specimens. However, the differences between groups were not statistically significant (p-value=0.687).
There was no significant relationship between PFS, OS and biological markers such as ki67 (p-value=0.950), p53 (p-value=0.752), MGMT promoter methylation (p-value=0.368) and 1p/19q deletion (p-value=0.379).
DISCUSSION
This study showed that the 6-month PFS was 20% and the median PFS was 2 months in recurrent and TMZ-refractory GBM patients treated with continuous low-dose TMZ chemotherapy. All patients had received radiotherapy with concomitant TMZ and cyclic TMZ therapy. Other cytotoxic agents or target therapies were not administered. In contrast to other trials using dose-dense or metronomic TMZ chemotherapy for recurrent GBM, tissue diagnosis was performed in 17 patients (56.7%) who underwent surgery. Fifteen specimens revealed recurrent GBM cells without radiation necrosis. Two patients with radiation necrosis with a few viable tumor cells showed 8 and 2 months of PFS following continuous low-dose TMZ therapy, respectively. In the case of treatment-related necrosis with tumor cells, deciding whether these tumor cells are still viable is difficult. It was reported that salvage pathologies reveal pseudoprogression (treatment-related necrosis without viable tumor cells) in 12 of 28 (42.8%) patients with GBM after concurrent radiotherapy and TMZ 26). Therefore, the investigators restricted entry into the clinical trial of recurrent GBM only to patients with disease progression for more than three months from the end of chemoradiation 21). We decided to give continuous low-dose TMZ to a patient with clinical deterioration previously treated with 6-cycle adjuvant TMZ chemotherapy following irradiation with concurrent TMZ, although the pathologic findings obtained by reoperation showed radiation necrosis with infiltration by a few tumor cells. It is suggested to consider surgery in clinically symptomatic patients, as it may improve the clinical condition of the patient and allow a histological diagnosis of the lesion (i.e., tumor or extensive necrosis, or both) 18). There are concerns that the response rate and antitumor effects of this regimen could be affected by pseudoprogression or radiation change. In the phase II RESCUE study (continuous TMZ 50 mg/m 2/d), 6-month PFS was 23.9% in recurrent GBM patients. Patients who had received prior chemotherapy for recurrent disease were excluded. Best response was shown in patients who had completed a prior course of concurrent TMZ chemoradiotherapy plus adjuvant TMZ followed by a drug-free period of at least 2 months 21). In the recent phase II trial study (continuous TMZ 50 mg/m 2/d), 6-month PFS was 19% and median OS was 7 months in recurrent GBM patients. Twenty-six patients (70%) had previously received bevacizumab or experimental targeted therapies. Patients with previous bevacizumab exposure survived significantly less than bevacizumab-naïve patients 20). Along with our results, continuous TMZ 50 mg/m 2/d protocol showed tolerable toxicities. Although grade III and IV hematologic toxicities did not occur in our series, lymphopenia is understood to be the most frequent toxicity experienced during therapy following this regimen. It was reported that microvessel density correlated significantly with postoperative survival in both previously untreated and treated patients with supratentorial astrocytomas 1,14). Microvessel density in high grade gliomas was significantly higher as compared to that in low grade gliomas. Microvessel density revealed a positive correlation with histologic grade in high grade gliomas 2,16). Initially, we investigated the relationship between the efficacy of continuous low-dose TMZ chemotherapy and the microvessel density of recurrent tumors. However, our series showed that microvessel density adds little information to help predict PFS and OS of recurrent GBM patients given continuous low-dose TMZ. It was stated that microvessel density may not be a predictor of treatment efficacy, because it is not a measure of the angiogenic dependence of a tumor, but rather reflects the metabolic burden of the supported tumor cells 8). Next, we compared microvessel density of recurrent specimens with that of the initial specimens. Interestingly, the microvessel density of recurrent specimens was significantly lower than that of the initial specimens. Changes in microvessel density reflect the changing ratio of the vascular component of the tumor to its tumor-cell component. Although a decrease in microvessel density is associated with the previous treatment, the disease status was identified as recurrence. This can be partially explained by the lower oxygen consumption rate of recurrent tumor cells. In addition, tumor cells are known to tolerate oxygen deprivation and to be resistant to apoptosis under hypoxic conditions 31). Because recurrent tumor cells can remain viable in low metabolic demand, the microvessel density in the recurrent specimen can be decreased. Although the small number of patients in this retrospective study is the major limitation, continuous low-dose TMZ does not influence GBM cells that develop the recurrence in poor angiogenic environments. Similarly, combination therapy with continuous low-dose TMZ and bevacizumab is not superior to TMZ only in terms of PFS and OS 28). The initial results reported at ASCO 2014 of the German randomized phase II DIREKTOR trial using the 'one week on-one week off' TMZ versus 'three weeks on-one week off' TMZ did not yield a significant difference between the two group 27). However, the analysis presented that MGMT promoter methylation status shows the same results as the study of Han et al. 7) : the 6-month PFS after dose-intensified TMZ was 39.7% in patients with methylated MGMT promoter versus 6.9% in patients without MGMT promoter methylation. In our series, there was no significant difference between MGMT promoter methylation status and the prognosis. Recently, other combination therapy beyond continuous low-dose TMZ only has been investigated for recurrent GBM 5,33).
CONCLUSION
Our findings show that continuous low-dose TMZ chemotherapy is not a promising alternative strategy for recurrent and TMZ-refractory GBM. Measurements of microvessel density do not have predictive value for recurrent GBM treated with continuous low-dose TMZ chemotherapy. It is critical to identify the resistance mechanism and develop novel strategies for the treatment of recurrent GBM.
References
1. Abdulrauf SI, Edvardsen K, Ho KL, Yang XY, Rock JP, Rosenblum ML : Vascular endothelial growth factor expression and vascular density as prognostic markers of survival in patients with low-grade astrocytoma. J Neurosurg 1998, 88 : 513-520,   2. Assimakopoulou M, Sotiropoulou-Bonikou G, Maraziotis T, Papadakis N, Varakis I : Microvessel density in brain tumors. Anticancer Res 1997, 17 : 4747-4753,  3. de la Taille A, Katz AE, Bagiella E, Buttyan R, Sharir S, Olsson CA, et al : Microvessel density as a predictor of PSA recurrence after radical prostatectomy. A comparison of CD34 and CD31. Am J Clin Pathol 2000, 113 : 555-562,   4. de Oliveira MV, Pereira Gomes EP, Pereira CS, de Souza LR, Barros LO, Mendes DC, et al : Prognostic value of microvessel density and p53 expression on the locoregional metastasis and survival of the patients with head and neck squamous cell carcinoma. Appl Immunohistochem Mol Morphol 2013, 21 : 444-451,   5. DI Cristofori A, Carrabba G, Lanfranchi G, Menghetti C, Rampini P, Caroli M : Continuous tamoxifen and dose-dense temozolomide in recurrent glioblastoma. Anticancer Res 2013, 33 : 3383-3389,  6. Franceschi E, Omuro AM, Lassman AB, Demopoulos A, Nolan C, Abrey LE : Salvage temozolomide for prior temozolomide responders. Cancer 2005, 104 : 2473-2476,   7. Han SJ, Rolston JD, Molinaro AM, Clarke JL, Prados MD, Chang SM, et al : Phase II trial of 7 days on/7 days off temozolmide for recurrent high-grade glioma. Neuro Oncol 2014, 16 : 1255-1262,    8. Hlatky L, Hahnfeldt P, Folkman J : Clinical application of antiangiogenic therapy : microvessel density, what it does and doesn't tell us. J Natl Cancer Inst 2002, 94 : 883-893,   9. Kerbel RS, Kamen BA : The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer 2004, 4 : 423-436,   10. Kieran MW, Turner CD, Rubin JB, Chi SN, Zimmerman MA, Chordas C, et al : A feasibility trial of antiangiogenic (metronomic) chemotherapy in pediatric patients with recurrent or progressive cancer. J Pediatr Hematol Oncol 2005, 27 : 573-581,   11. Ko KK, Lee ES, Joe YA, Hong YK : Metronomic treatment of temozolomide increases anti-angiogenicity accompanied by down-regulated O(6)-methylguanine-DNA methyltransferase expression in endothelial cells. Exp Ther Med 2011, 2 : 343-348,    12. Kreisl TN, Kim L, Moore K, Duic P, Royce C, Stroud I, et al : Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 2009, 27 : 740-745,   13. Kyritsis AP, Levin VA : An algorithm for chemotherapy treatment of recurrent glioma patients after temozolomide failure in the general oncology setting. Cancer Chemother Pharmacol 2011, 67 : 971-983,   14. Leon SP, Folkerth RD, Black PM : Microvessel density is a prognostic indicator for patients with astroglial brain tumors. Cancer 1996, 77 : 362-372,   15. Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG : Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 1990, 8 : 1277-1280,   16. Mahzouni P, Mohammadizadeh F, Mougouei K, Moghaddam NA, Chehrei A, Mesbah A : Determining the relationship between "microvessel density" and different grades of astrocytoma based on immunohistochemistry for "factor VIII-related antigen" (von Willebrand factor) expression in tumor microvessels. Indian J Pathol Microbiol 2010, 53 : 605-610,   17. Meert AP, Paesmans M, Martin B, Delmotte P, Berghmans T, Verdebout JM, et al : The role of microvessel density on the survival of patients with lung cancer : a systematic review of the literature with meta-analysis. Br J Cancer 2002, 87 : 694-701,    18. Mou YG, Sai K, Wang ZN, Zhang XH, Lu YC, Wei DN, et al : Surgical management of radiation-induced temporal lobe necrosis in patients with nasopharyngeal carcinoma : report of 14 cases. Head Neck 2011, 33 : 1493-1500,   19. Murri AM, Hilmy M, Bell J, Wilson C, McNicol AM, Lannigan A, et al : The relationship between the systemic inflammatory response, tumour proliferative activity, T-lymphocytic and macrophage infiltration, microvessel density and survival in patients with primary operable breast cancer. Br J Cancer 2008, 99 : 1013-1019,    20. Omuro A, Chan TA, Abrey LE, Khasraw M, Reiner AS, Kaley TJ, et al : Phase II trial of continuous low-dose temozolomide for patients with recurrent malignant glioma. Neuro Oncol 2013, 15 : 242-250,   21. Perry JR, B├®langer K, Mason WP, Fulton D, Kavan P, Easaw J, et al : Phase II trial of continuous dose-intense temozolomide in recurrent malignant glioma : RESCUE study. J Clin Oncol 2010, 28 : 2051-2057,   22. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al : Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005, 352 : 987-996,   23. Taal W, Segers-van Rijn JM, Kros JM, van Heuvel I, van der Rijt CC, Bromberg JE, et al : Dose dense 1 week on/1 week off temozolomide in recurrent glioma : a retrospective study. J Neurooncol 2012, 108 : 195-200,    24. Tanaka F, Otake Y, Yanagihara K, Kawano Y, Miyahara R, Li M, et al : Evaluation of angiogenesis in non-small cell lung cancer : comparison between anti-CD34 antibody and anti-CD105 antibody. Clin Cancer Res 2001, 7 : 3410-3415,  25. Tolcher AW, Gerson SL, Denis L, Geyer C, Hammond LA, Patnaik A, et al : Marked inactivation of O6-alkylguanine-DNA alkyltransferase activity with protracted temozolomide schedules. Br J Cancer 2003, 88 : 1004-1011,    26. Topkan E, Topuk S, Oymak E, Parlak C, Pehlivan B : Pseudoprogression in patients with glioblastoma multiforme after concurrent radiotherapy and temozolomide. Am J Clin Oncol 2012, 35 : 284-289,   27. van den Bent MJ, Taal W : Are we done with dose-intense temozolomide in recurrent glioblastoma? Neuro Oncol 2014, 16 : 1161-1163,    28. Verhoeff JJ, Lavini C, van Linde ME, Stalpers LJ, Majoie CB, Reijneveld JC, et al : Bevacizumab and dose-intense temozolomide in recurrent high-grade glioma. Ann Oncol 2010, 21 : 1723-1727,   29. Wick A, Felsberg J, Steinbach JP, Herrlinger U, Platten M, Blaschke B, et al : Efficacy and tolerability of temozolomide in an alternating weekly regimen in patients with recurrent glioma. J Clin Oncol 2007, 25 : 3357-3361,   30. Wick W, Platten M, Weller M : New (alternative) temozolomide regimens for the treatment of glioma. Neuro Oncol 2009, 11 : 69-79,    31. Yang L, Lin C, Wang L, Guo H, Wang X : Hypoxia and hypoxia-inducible factors in glioblastoma multiforme progression and therapeutic implications. Exp Cell Res 2012, 318 : 2417-2426,   32. Yang SH, Hong YK, Yoon SC, Kim BS, Lee YS, Lee TK, et al : Radiotherapy plus concurrent and adjuvant procarbazine, lomustine, and vincristine chemotherapy for patients with malignant glioma. Oncol Rep 2007, 17 : 1359-1364,   33. Zustovich F, Landi L, Lombardi G, Porta C, Galli L, Fontana A, et al : Sorafenib plus daily low-dose temozolomide for relapsed glioblastoma : a phase II study. Anticancer Res 2013, 33 : 3487-3494,  
Fig.┬Ā1
Glioblastoma with necrosis and hyaline thickening of vascular walls associated with radiation (A) hematoxylin & eosin (H&E) (├Ś100). Area of radiation necrosis (B) (├Ś200) with infiltration of viable tumor cells (arrow) (C) having Ki-67 positivity (D) (├Ś400).
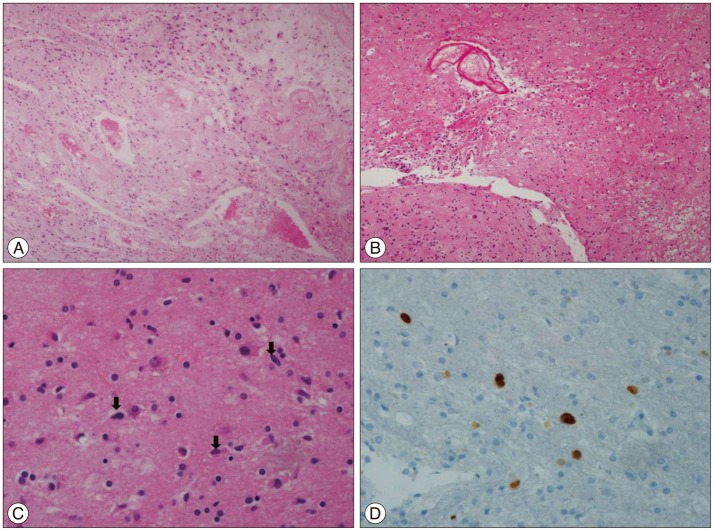
Fig.┬Ā2
Kaplan-Meier curves showing progression-free survival (PFS) (A) and overall survival (OS) (B).
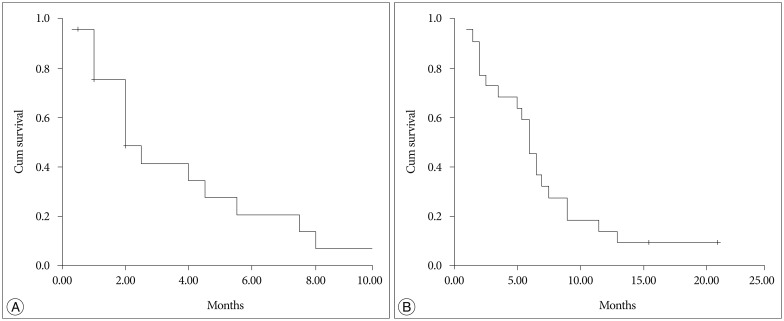
Fig.┬Ā3
Vessels stained with cluster determinant 34 and a light counterstain of hematoxylin. Magnification : ├Ś200. Area of low (A) and high (B) microvessel density.
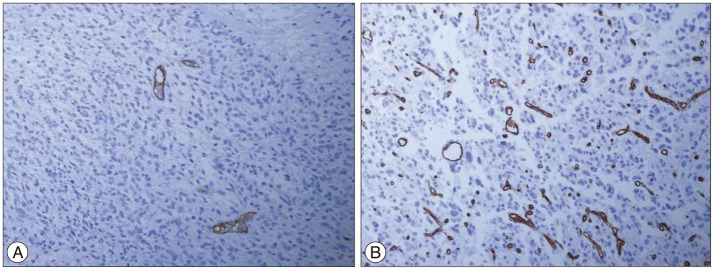
Fig.┬Ā4
Kaplan-Meier curves of progression-free survival (A) and overall survival (B) according to microvessel density within the recurrent tumors (p-value : 0.144, 0.156, respectively). MVD : microvessel density.
Table┬Ā1
Patient characteristics
|
|