INTRODUCTION
Many conventional and traditional vascular operations are performed during neurosurgery. However, neuroendovascular treatment (NET) is emerging as a separate alternative treatment. NET began as a hybrid of traditional neurosurgical and neuroradiological approaches and is now widely used clinically for many therapeutic indications. Given the increasing importance of NET in neurovascular surgery, neurosurgeons are encouraged to become trained in NET. Transfemoral catheter angiography (TFCA) is a basic NET procedure, and it is also considered an important diagnostic modality for neurovascular diseases.
As the number of NET procedures performed by neurosurgeons increases, resident neurosurgeons have many opportunities to participate in NET procedures. Unfortunately, it is difficult for neurosurgical residents to train in TFCA in most neurosurgery departments, and NET training guidelines for fellowships or residencies have not been established in Korea. TFCA training should be essential for neurosurgical residents because many neurosurgeons are required to perform TFCA. It is also commonly performed as a basic procedure of NET and is a diagnostic gold standard. Appropriate training and abundant experience are keys to performing safe TFCA procedures.
Resident neurosurgeons had the opportunity to train in TFCA at our hospital, and this paper presents the results of TFCA training using our standard protocol.
MATERIALS AND METHODS
A senior resident neurosurgeon was trained in TFCA from May 1 to September 31, 2011, performing 112 consecutive TFCAs under the supervision of two neuroendovascular specialists. All TFCA procedures were performed in the angiography suite. Patient demographic data, TFCA indications, side of approach, number of arteries selected, and complications were analyzed.
TFCA protocol
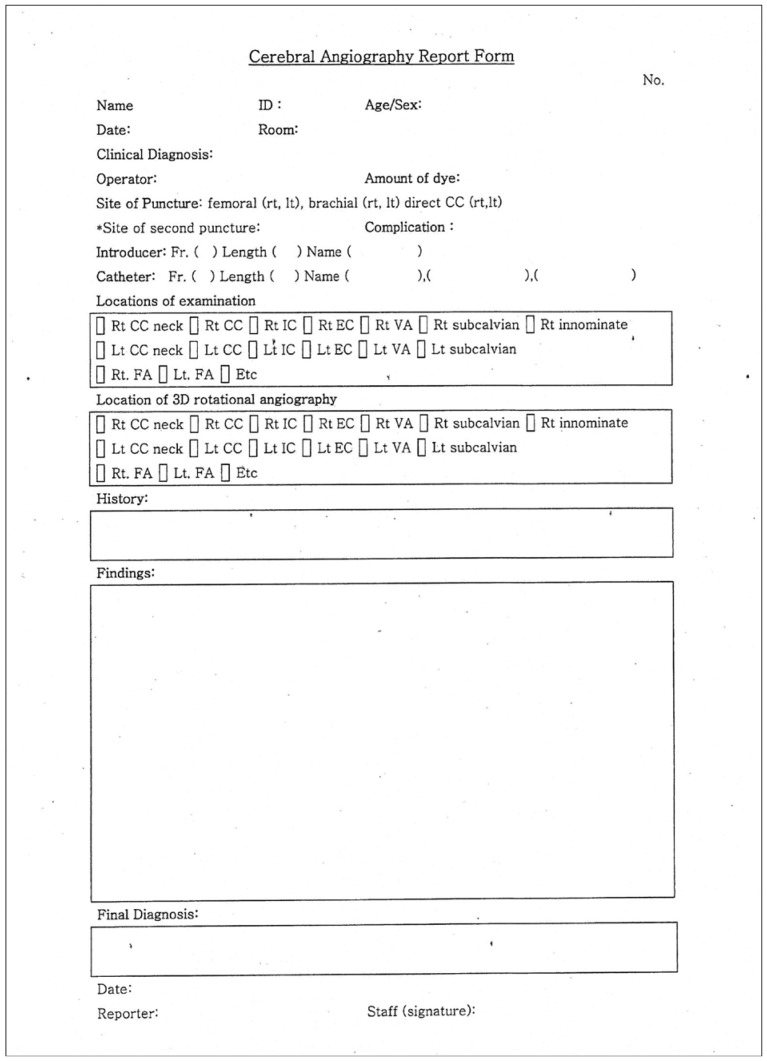
The standard protocol was established based on our previously published cadaveric anatomy study of the inguinal area and aortic arch11,17). In the process of designing the training protocol, we designated patient safety as a top priority. Standardized TFCA protocols of our neurosurgical institute are as follows. 1) The operator should fully understand the neurovascular anatomy of the inguinal area and the configuration of the aortic arch and its major branches, which were previously published in our cadaveric studies. 2) The anterior wall of the femoral artery is punctured at the level of the bottom of the femoral head with the Seldinger technique, and femoral arteriography is performed at an oblique angle of 25° at the site of femoral puncture. 3) 5 Fr catheters are used in adult patients, and 4 Fr catheters are used for patients under the age of 10 years. The catheter techniques are performed as gently as possible, as in microneurosurgery. 4) Selective catheterization of the carotids (internal, external), vertebral, or subclavian arteries is usually performed. 5) Road map images are taken at every step of the selective catheterizations, especially in the tortuous orifices and curvatures of the vertebral artery. 6) A 100-cm Davis diagnostic catheter (Cook Medical, Bloomington, IN, USA) is initially used. If this fails, a 100-cm Headhunter catheter (Cook Medical) and 100-cm Simon catheter (Cook Medical) are used in sequence depending on the complexity of the aortic arch and the configuration of its major branches. 7) Catheters are positioned as proximally as possible (that is, in the largest caliber of the selected artery) within the range of adequate diagnosis. 8) During vertebral angiography, if a catheter is unstable at the orifice due to the tortuosity, contrast dye is injected by hand. 9) If the operator fails to select the target vessel with a catheter, the supervisor becomes directly involved in the procedure or declares an end to the procedure. 10) Intracranial angiography is performed on the common carotid artery in the case of Moyamoya disease. 11) The operator should be fully aware of the constant dye concentration (100 mL of dye mixed with 40 mL of N/S), injection speed, and volume (5 mL/sec and 7-mL volume in the internal carotid; 4 mL/sec and 6-mL volume in the vertebral artery). 12) The femoral sheath is removed immediately after completion of angiography, and manual compression is applied for 20 minutes to achieve hemostasis. 13) The operator should complete the Cerebral Angiography Report Form after the procedure and then receive confirmation from the supervisor (Fig. 1).
RESULTS
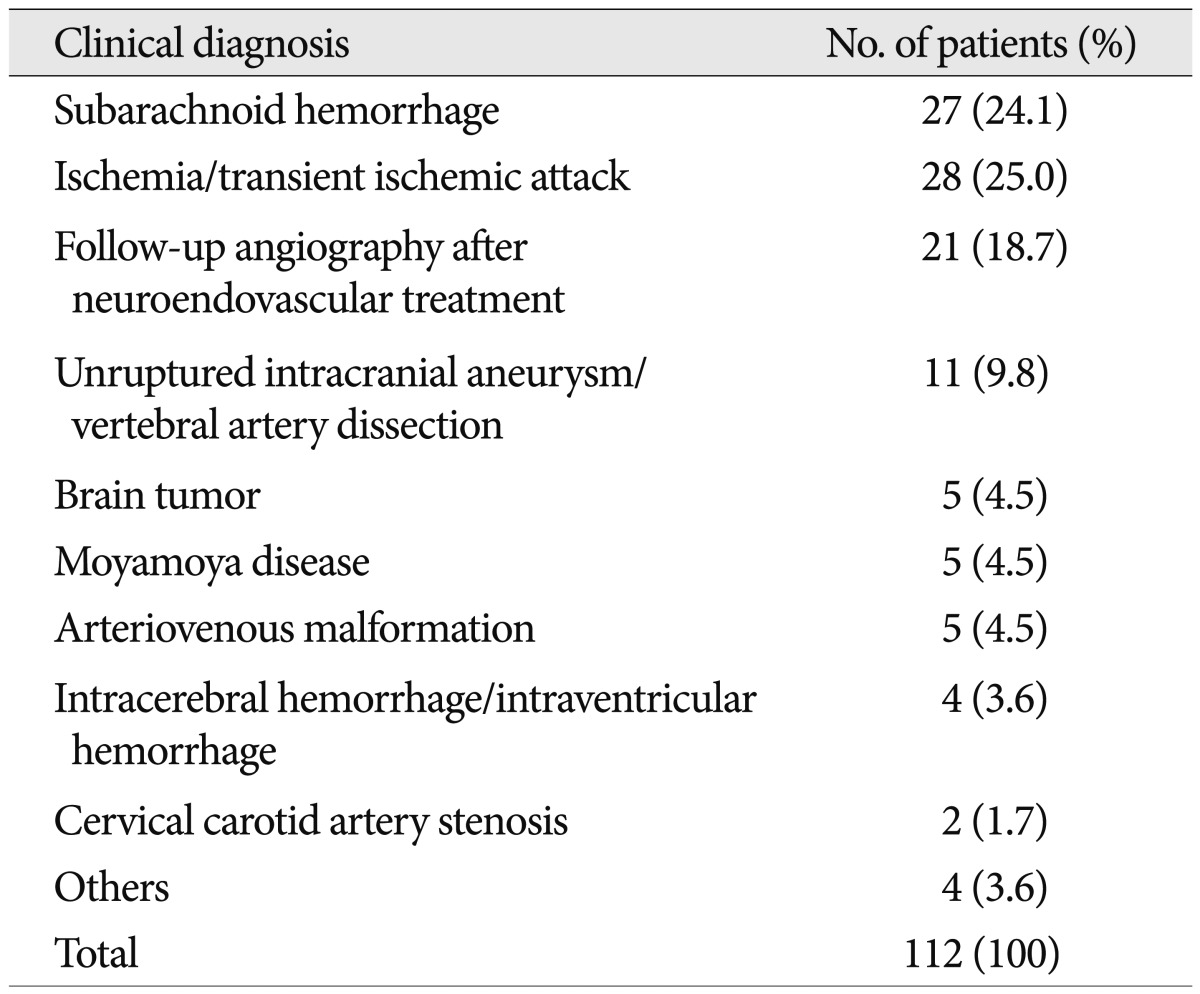
A total of 64 males and 48 females underwent TFCA by a senior resident neurosurgeon. The mean patient age was 51.6 (range 12-80) years. Twenty-seven patients were diagnosed with subarachnoid hemorrhage, and 28 had ischemia or a transient ischemic attack. Twenty-one patients were included in a follow-up study after coil embolization or clip operation for aneurysms. Eleven patients had unruptured intracranial aneurysms or vertebral artery dissection. Five patients each had a brain tumor, Moyamoya disease, and arteriovenous malformation. Four patients had intracerebral hemorrhage or intraventricular hemorrhage, two had cervical carotid artery stenosis, and four patients had other conditions (Table 1).
Puncture site
All procedures involved the femoral access route. A total of 110 patients underwent puncture of the right femoral artery, and two underwent puncture of the left femoral artery.
Catheters
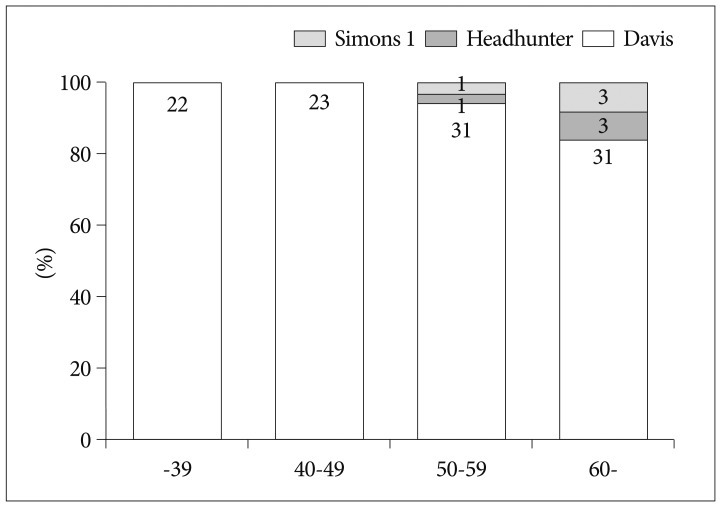
The Davis catheter was initially chosen for all patients. However, it was replaced with a Headhunter or Simons catheter when the operator failed to select the target vessel with the Davis catheter. A total of 45 patients <49 years of age were treated with only a Davis catheter. TFCA was performed on 31 patients 50 to 59 years of age. A Davis catheter was used in 30 of these patients, and Davis, Headhunter, and Simons catheters were used in one patient. Twenty-eight patients >60 years of age were treated with only a Davis catheter. Two types of catheters were used in three patients, and three types were used in one patient (Fig. 2).
Number of vessels selected in angiography
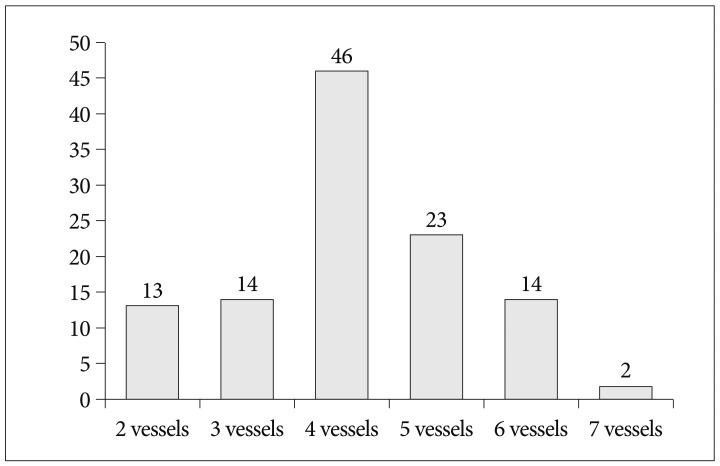
Selected vessels included the femoral artery, common carotid artery in the neck, intracranial carotid artery, external carotid artery, vertebral artery, subclavian artery, and aorta. Femoral artery angiography was performed in all patients to check for puncture site complications after the femoral sheath was inserted. Two-vessel angiography was performed in 13 patients and three-vessel angiography in 14 patients. Four vessels were selected in 46 patients, and five vessels in 23 patients. Six-vessel angiography was performed in 14 patients, and seven-vessel angiography was performed in two patients (Fig. 3). A total of 465 selective vessel angiography procedures were performed in 112 patients who underwent TFCA without complications. The mean number of angiography procedures was 4.14 vessels per patient.
DISCUSSION
Despite the recent advances in noninvasive diagnostic neuroimaging, diagnostic cerebral angiography is still the cornerstone and gold standard for evaluations and treatment of cerebrovascular disease3). In addition to a high level of technical expertise, performance and interpretation of diagnostic cerebral angiography requires profound cognitive knowledge of related neurological pathophysiology and neurovascular anatomy and pathology as well as an understanding of the full range of neurodiagnostic possibilities. Expertise in diagnostic cerebral angiography is the foundation of safe and successful neuroendovascular interventions such as carotid artery angioplasty and stenting for atherosclerosis, interventional stroke therapy, intracranial angioplasty and stenting, and embolization of cerebral aneurysms, epistaxis, and vascular malformations4).
Formal neuroscience education, adequate procedural training, and sufficient experience are all essential to ensure desirable outcomes and to gain a high level of competence in diagnostic cerebral angiography and interventional procedures. The United States, Europe, and Japan have guidelines or educational programs for NET training4), whereas the Korean Neurosurgical Society and Society of Korean Endovascular Neurosurgeons do not.
Endovascular procedures are prone to causing strokes, leaving patients with problematic sequelae. Owing to the risk for procedure-induced stroke, many physicians do not recommend this procedure, and some patients become reluctant to undergo this procedure3,18). The risk for permanent neurological deficits caused by diagnostic cerebral angiography is considerable and ranges from 0.3 to 5.7%7,10,12,13,15). Experienced neurovascular specialists can have complication rates lower than 1%9). There is an additional risk for temporary neurological deficits ranging from 0.3% to 6.8%, which means that the risk is increased two to three fold on average compared with the risk for permanent neurological deficits7,10,12,13,15). Patients with atherosclerotic cerebrovascular disease manifested by neurological symptoms (transient ischemic attack or stroke) have a risk for stroke from diagnostic cerebral angiography that is two- to three-fold that of patients with asymptomatic lesions5). These findings explain the emphasis on a strictly systematic education for NET, and the importance of formal education programs for patient safety cannot be overemphasized.
A senior resident neurosurgeon participated in NET as an assistant and performed DSA under supervision in our institute. NET education of a senior resident neurosurgeon has some advantages in neurosurgical education. 1) It helps improve the understanding of neurovascular disease. 2) It helps to acquire a technical base for NET. 3) It helps to gain knowledge about neuroradiology and radiophysiology. 4) Senior resident neurosurgeons are capable of managing patients with neurovascular disease and can improve their abilities related to treatment decisions, planning, and preprocedural care by participating in diagnostic procedures.
Most countries recommend that NET programs should only be available to board-certified neurosurgeons or radiologists1,8,9,16) because NET is a subspecialty of neurosurgery or radiology, and trainees need enough experience to handle neurosurgical disease before NET training. According to an analysis of 5000 angiogram cases, fellowship-trained specialists have fewer neurological complications (0.5%) than do even experienced angiographers (0.6%), and both have far fewer complications than trainees under supervision (2.8%)12-14). However, there is no doubt that every trainee has a starting point and that no one can be an expert from the beginning. Moreover, senior neurosurgical residents have enough experience in neurosurgical disease management to perform NET. Therefore, they benefit from an opportunity to learn the basic procedures of NET and improve their knowledge of neurosurgical disease.
The most important factor in resident training is access to adequate cases that encompass a range of cerebrovascular diseases. Many guidelines of NET training have recommended 100 or more diagnostic angiograms before starting training in endovascular procedures, such as embolization of aneurysms, arteriovenous malformations and tumors, angioplasty and stenting for the treatment of intracranial and extracranial occlusive cerebrovascular disease, and the performance of invasive functional testing2,6,8). However, resident training courses have not focused on treatment skills in endovascular procedures. Assistance roles and performance of TFCA procedures are enough to learn endovascular treatments that are part of neurovascular treatment modalities. Moreover, the recommended number of 100 or more diagnostic angiograms is always arbitrary. In any surgical procedure, some residents or fellows are ready to perform procedures quickly, while others need many more repetitions before gaining competence6).
With improvements in noninvasive imaging modalities of the cerebral vasculature, the indications for diagnostic angiography will decrease, making it increasingly difficult to achieve the designated number of 100 diagnostic angiograms and to enter the field of NET. It is necessary to start NET training early during a residency. In our experience, senior residents have already fulfilled the number of recommended digital subtraction angiographies during their residency. Therefore, with enough experience and cases, they will be able to focus more on treatment procedures during their fellowship.
Because patient safety is the top priority in TFCA training, it was considered to be most important in our institute's training guidelines. Resident neurosurgeons should understand the anatomy of the inguinal area and aortic arch before TFCA procedure training. The TFCA training protocol was established on the following principle: "Do not do more than trainees can handle during TFCA". In particular, when it comes to selective dye injection, the protocol is designed to be performed in the proximal part of vessels, which is a good option for patients who have unstable cerebral vascular hemodynamics such as that caused by cervical internal carotid artery stenosis and Moyamoya disease. Patients with these diseases showed instability of cerebral vascular hemodynamics, and selective dye injection was performed on the common carotid artery. This action helped to avoid manipulation of the internal carotid artery and decrease hemodynamic stress, although the amount of dye increased more in common carotid artery angiography than in internal carotid artery angiography.
An endovascular specialist was involved the TFCA performed during the senior resident training when; 1) vessel selection was difficult for the resident neurosurgeon, 2) multiple catheters were used because of vessel tortuosity, 3) better TFCA skills were needed to avoid complications in elderly patients or those with unstable disease, 4) the resident neurosurgeon was confused by the anatomical variation of the vessels, or 5) the femoral artery puncture failed despite multiple attempts. The supervisor pointed out the errors of the resident neurosurgeon during training. The main errors were as follows: the trainee 1) advanced the diagnostic catheter and guidewire with too much force and too quickly, 2) did not check for an air bubble in the injection syringe, 3) advanced the diagnostic catheter and guidewire outside the image, and 4) did not confirm blood regurgitation before connecting the dye injector.
Although the senior resident did not experience complications in this series, complication care is as important as avoiding complications. It is important that the trainee does not panic and does ask a supervisor for help. In this way, the trainee will learn to manage complications while resolving complications with a supervisor.
This study has some limitations. First, it was retrospective and did not compare groups. Second, it was a single-center experience, and the results cannot be generalized to all TFCA training. Prospective multicenter trials are needed. Nevertheless, the study shows that a resident neurosurgeon was capable of safely performing 112 consecutive TFCA procedures under the supervision of experienced endovascular specialists.