An and Hyun: Pediatric Spine Trauma
Abstract
Pediatric spine has growth potential with incomplete ossification, and also unique biomechanics which have important implications for trauma patients. This article intends to review various aspects of pediatric spine trauma including epidemiology, anatomy and biomechanics, and clinically relevant details of each type of injury based on the location and mechanism of injury. With the appropriate but not superfluous treatment, pediatric spine trauma patients can have better chance of recovery. Therefore, as a spine surgeon, understanding the general concept for each injury subtype together with the debate and progress in the field is inevitable.
Key Words: Pediatrics ┬Ę Trauma ┬Ę Spinal injuries ┬Ę Craniocervical injuries ┬Ę Neurocentral junction.
EPIDEMIOLOGY
Spinal column and/or spinal cord trauma patients can present within full spectrum from mild to disabling injury, and even death. According to the numerous data from foreign references, of which the majority from USA, pediatric spine trauma is infrequent, known to be only about 2% to 5% of all spinal injuries [ 13], and 60% to 80% of them involves cervical spine largely due to the anatomy and biomechanics of those specific age group [ 81]. Pediatric thoracolumbar spine fractures mainly occur during adolescent age of 14 to 16 [ 14]. The predominant mechanism of injury for younger children (0 to 9 years of age) is falls and pedestrian-to-automobile accidents, whereas for older children (10 to 18 years of age) automobile accidents prevail [ 88]. Child abuse is another noteworthy cause of pediatric spine injury, as cases are expected to increase and initial active involvement is crucial. Korean Statistical Information Service reports that child abuse cases are escalating yearly, and its detailed national report on year 2017 revealed that 2.64% of whole pediatric population was reported to be abused, with physical abuse involvement accounts for almost 40% of all cases [ 54]. Several USA studies showed that child abuse account for less than 1% of all pediatric spine injuries [ 44], and skeletal survey for suspected child abuse revealed that about 10% of them had spinal fractures [ 5]. Regarding spinal cord injury (SCI), neonatal patients are associated with obstetrical manipulation, with the incidence of one in 80000 live births [ 81], and there is a bimodal peak age group for young adults and adolescents as a first peak and geriatrics as a second peak, with the rough incidence of 115 and 800 per 1 million, respectively [ 44, 45, 92].
PEDIATRIC SPINE ANATOMY, BIOMECHANICS, AND DEVELOPMENT
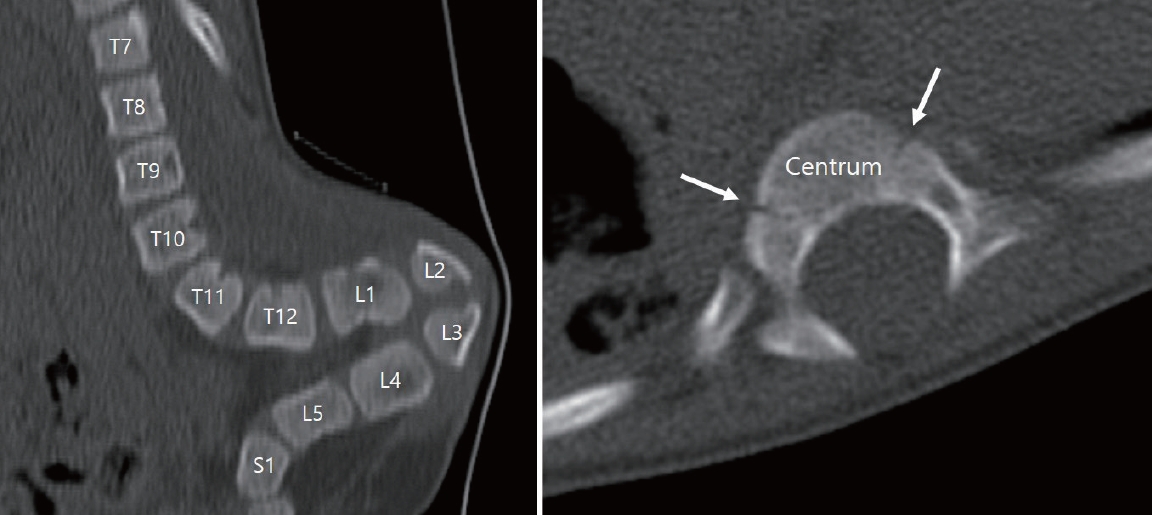
Children have unique spinal anatomy and biomechanics that contributes to various features of pediatric spine trauma. One neonatal cadaver study revealed that neonatal vertebral column can stretch as much as 2 inches without disruption, but the spinal cord can only stretch 0.25 inches [ 59]. This bony column flexibility stems from inherently flexible and elastic pediatric spinal ligaments and joints. Specifically, facet joints are smaller, more horizontally oriented and shallower than adults which allow for more translation during spine movement with less stability. Absent uncinate process until age of 10 adds additional mobility to the cervical spine as this structure limits lateral and rotational movements. Spinal ligaments and joint capsules are able to stretch without disruption of tissue due to the higher water content. These biomechanics combined with the relatively stiff spinal cord accounts for higher rates of SCI without radiographic abnormality (SCIWORA) of all pediatric spine injuries compared with adults reported in multiple studies [ 6, 30, 88]. Another important feature for children under age 8 is that their head is relatively heavy and large compared with their body. This high head-to-torso ratio makes neck in relatively flexed position compared to adults [ 96] with the fulcrum of flexion at C2-C3 in infants, C3-C4 by age 5, C4-C5 at age 10, and C5-C6 by age 15 [ 9, 52]. These features account for the finding that upper cervical injury predominates for children under the age 8 [ 70]. Ossification process is an important part of pediatric spinal development which affects trauma pattern and radiographic findings. One noticeable finding is the neurocentral junction (NCJ), which is the synchondroses between developing vertebral body (centrum) and vertebral arch ( Fig. 1), subsequently begins to fuse at the age 3-6, becoming the physeal scar in adult spine [ 64]. Surgical implication of NCJ is that as a persistent plate of bone inside every vertebral body throughout life, it is recommendable to be traversed when inserting pedicle screw to get additional support and avoid loosening [ 64]. Other relevant pediatric spine features are as follows. Initially cartilaginous C1 body at birth is radiographically not visible until the age 1, spinous processesŌĆÖ synchondroses at midline fuses at age 3. At the age of 3-6 years, NCJ and synchondrosis between odontoid and body of C2 fuse, with ossification center appearing at the tip of the odontoid, and the anterior wedging of vertebral bodies resolve. Upper cervical spine pseudosubluxation and widening of predental space resolves by age 8. At puberty, superior and inferior epiphyseal rings together with secondary ossification centers at the tip of spinous processes appear and summit ossification center of odontoid fuses. Secondary ossification centers fuse roughly by the age 25. Epiphyseal injury should be always kept in mind as consequent premature epiphyseal fusion can lead to deformity and affect growth, which is difficult to detect initially from plain radiograph. SharpeyŌĆÖs fibers exist at the periphery of annulus fibrosus and insert into adjacent superior and inferior epiphyseal rings. The strength of this fiber exceeds that of attachment of epiphyseal rings and vertebrae, and this accounts for the detachment of epiphyseal rings from vertebrae with shearing force [ 52].
PEDIATRIC CERVICAL SPINE TRAUMA
Cervical spine injury comprises most of the pediatric spine injury which makes the categorical review invaluable. Younger children below age 10 have relatively heavy head and are subject to high-velocity pedestrian accident, which makes them vulnerable to craniovertebral junction (CVJ) injuries, which are classified and reviewed in detail. Conversely, older children have spinal injury pattern similar to adults mostly at subaxial spine with less involvement of CVJ. The Congress of Neurological Surgeons have published a guideline for imaging surveillance for pediatric trauma patients to clear cervical spine [ 85]. It suggests cervical spine anteroposterior and lateral X-rays or high-resolution computed tomography (CT) to pediatric trauma patients with difficulty in communication, neurologic deficit, neck pain, distracting pain, intoxication, or high energy injury mechanism. In addition, open-mouth view is not recommended for children under age 9, and CT over X-ray is recommended for suspected atlantooccipital dislocation (AOD). Algorithm provided by Pediatric Cervical Spine Clearance Working Group is similar to some extent, utilizing Glasgow coma scale, trauma history, and physical exam findings for the decision to carry out surveillance X-ray or CT [ 39].
CVJ injuries
CVJ is the most mobile segment of spine which consists of occiput, atlas, and axis. Grossly 2 segments comprise CVJ : atlantooccipital segment and atlantoaxial segment. Each segment has its own ligaments which stabilize and allow specific motion. And several extrinsic ligaments that are not specific to CVJ but contiguous to the other parts of spine function as stabilizers. The atlanto-occipital segment allows 23┬░ to 24.5┬░ of flexion/extension and 3.4┬░ to 5.5┬░ lateral bending of the cranium. Among cervical spinal rotational capacity of 90┬░, atlantoaxial segment contributes the most (25┬░ to 30┬░), with flexion/extension capacity of 10.1┬░ to 22.4┬░ [ 77]. Supraphysiological motion or excess force applied to CVJ can cause various types of injuries.
AOD
Although rare, younger children below age 10 are vulnerable to this type of injury due to relatively heavy head and smaller, horizontally oriented atlantooccipital joints [ 52] which makes CVJ vulnerable to shearing forces. Fatal AOD cases are found to have widespread ligamentous disruption, especially alar ligament and tectorial membrane [ 2]. Clinical presentation is variable, including neck pain, low cranial nerve deficit, extremity weakness, and even death [ 36]. Radiographic diagnostic criteria is not clearly defined for AOD, as none of the single available method is perfect [ 50]. The Traynelis classification divides AOD into three groups [ 95] : anterior displacement is type I, axial distraction is type II, posterior displacement is type III, but this method overlooks coronal malalignment [ 36]. PowersŌĆÖ ratio measured at the midsagittal plane compares distance from basion to anterior cortex of posterior arch of atlas with distance from opisthion to posterior cortex of anterior arch of atlas [ 82]. Normal value is less than 0.9, with higher values represent type I AOD, but is less sensitive for type II or III AODs. The X-line method, which is more sensitive than powersŌĆÖ ratio in detecting Traynelis type II and III AODs, draws two lines at midsagittal plane and assess anatomical relationship of CVJ [ 57]. Measuring basion-dens interval and basion-axis interval is the other way to detect AOD, and Harris method utilizes these two measurements collectively [ 37, 38]. Lastly, occipital condyleC1 interval measurement is specific for Traynelis type II injuries, and is validated in pediatric population. As above, AOD presents clinically and radiographically diverse which makes clinicianŌĆÖs high index of suspicion important for diagnosis and prevention of secondary injury. Prompt cervical immobilization, hemodynamic management and early aggressive surgical stabilization is crucial for better outcome. Traction is generally avoided due to the risk of neurological deterioration [ 94]. Halo fixation use is declining these days due to its ineffectiveness in immobilization and potential for morbidity [ 80], combined with the AODŌĆÖs lack of ability for spontaneous healing [ 35]. Posterior fixation is more useful for AOD than anterior fixation to achieve surgical treatment with O/C1, O-C2, or O-C2 without C1 fusion. Former wiring techniques are mostly replaced with various screw fixation techniques including transarticular, lateral mass, C2 pedicle, or laminar screws [ 36].
Atlantoaxial rotatory subluxation (AARS)
The atlantoaxial joint is mainly stabilized by transverse ligament and alar ligaments and has harmonious biomechanical relationship during rotatory movement [ 74]. Transverse ligament limits excessive anterior translation of atlas on axis, and alar ligaments limit excessive rotation of atlas. Injury of these ligaments due to various mechanisms lead to atlantoaxial joint instability. Atlantoaxial rotatory displacement (AARD), AARS, and atlantoaxial rotatory fixation (AARF) are terms used to describe a spectrum of atlantoaxial joint rotational abnormality [ 7, 74- 76]. Sometimes the terms AARD, AARS, and AARF are intermixed, and torticollis is mistakenly regarded as same as AARD, despite being a separate entity [ 33]. For the umbrella term for three spectrums of condition, AARS is used in this article. There are various pathologies (infection, head/cervical operation, major/minor trauma, genetic disease) associated with AARS, but culprit biomechanical cause of fixation, or locking of the atlantoaxial joint followed by subluxation/dislocation is not fully understood [ 33]. AARS clinically presents with neck pain and discomfort, limited rotation, typically cock-robin deformity with neck rotated in one direction and tilted in the opposite direction, and rarely neurologic symptoms. Diagnosis is difficult to attain radiographically as simple radiography is not fully diagnostic, and even standard or dynamic CT can be misleading [ 72]. Due to the inability to retain neutral head position, bony relationships are obscured by soft tissue in plain radiograph. Although CT is a valuable tool to investigate static joint relationship of atlas and axis, it does not represent dynamic relationship. For this reason, some advocate the use of dynamic CT, but there are also concerns about the reproducibility and its diagnostic value [ 73, 75]. Magnetic resonance imaging (MRI) can reveal joint capsule or ligamentous edema, surrounding soft tissue pathology or cord injury, but has little implication in treatment decision so far. Therefore, diagnosis of AARS is primary a clinical one, aided by multiple imaging modalities. Torticollis and AARD can be distinguished by the side of the sternomastoid spasm, as torticollis shows contralateral spasm relative to the side of the chin, but AARD shows the opposite. Fielding and Hawkins presented classification of AARF based on the degree and direction of displacement of atlas, utilizing static CT with head position as initial presentation [ 31]. Various treatment algorithms are presented in literatures with no consensus. As AARS is a clinical diagnosis, some patients will fall into diagnostic grey zone, and they are treated conservatively with/without collar/brace [ 76]. Many studies classify patients as acute, chronic, and congenital based on the duration of symptom for treatment modality decision purpose, but the cut-off point for acute/chronic is variable. Acute AARS is generally considered benign, treated with less invasive closed reduction such as halter traction, followed by external immobilization or immobilization alone with good clinical outcome [ 66, 69]. Persistent acute AARS cases together with chronic/congenital cases require either longer/repeated closed reduction, or more invasive traction devices such as Gardner-Wells-style tongs or halo vest but there is no consensus upon traction and stabilization period, the number of attempts before considered irreducible, and the type of traction device of choice [ 66, 69, 73, 75]. Generally, irreducible cases require operative stabilization for C1/C2.
Translational atlantoaxial subluxation (TAAS)
Translation of atlantoaxial joint is limited by intact odontoid process, C1/2 joint capsule and disc, and associated ligaments [ 83]. Violent trauma, hyperextension, or distraction injury can cause traumatic TAAS [ 52, 67, 82]. Nontraumatic cases can also arise from inflammation, facet tropism, spinal tumors, or congenital disorders including spinal fusion, Down syndrome and skeletal dysplasias [ 1, 52, 62, 86]. Clinical presentation is diverse, from minor neck pain to myelopathy due to cord compression or cerebellar/occipital lobe infarction due to vertebral artery stenosis [ 8, 32, 89]. Compared with AARS, radiographic diagnosis of TAAS is relatively straightforward as slippage of atlantoaxial facet is easily identified from coronal/sagittal plane of CT image, with several proposed classification systems for translational subluxation itself or transverse ligament injury [ 23, 61, 63]. Noninvasive immobilization can be attempted, but extensive ligamentous injury or neurologic complication is an indication for C1/2 fusion operation [ 52].
CVJ fractures
Occipital condyle fracture (OCF), although being rare, should be considered when evaluating high impact head trauma patient, including automobile and sports accidents. Associated injuries including intra and extra-axial lesions need to be investigated due to the nature of the mechanism of injury. Neurologically, the patient can present from normal finding to brainstem, cord, or cranial nerve deficit. Neurologic instability comes from direct neural compression by avulsion of the fractured segment, or cord contusion without bony fragment displacement [ 15]. Radiographically, OCF is difficult to detect from plain film, so thin section CT is recommended for diagnosis. Some suspect that OCF is underdiagnosed due to the difficulty of diagnosis [ 15, 22]. OCF might cause instability of CVJ due to the attached ligaments at occipital condyle, especially when the alar ligaments are coaffected [ 4]. The general principle of OCF management is conservative with stable CVJ, and occipitocervical fusion with CVJ instability [ 71]. Pediatric atlas fracture is rarely reported with consistent mechanism of injury of fall from vertex or automobile accident. It is important to note lateral pseudospread, a normal variant of atlas due to the initial fast growth than axis, and three synchondroses which can be confused with true fractures. For isolated atlas fracture, conservative treatment is reported to be sufficient with full functional recovery [ 46]. Younger children has odontoid fractures at neurocentral synchondrosis which is known to fuse by age 5 to 7, and older children has true adult type odontoid fractures [ 52]. Most of the patients will not experience neurologic deficits. Resultant widening of odontoid epiphysis can be visualized by CT or MRI. Conservative management is considered without marked displacement of odontoid process and is applicable to most of the cases [ 29, 68]. Operative osteosynthesis of dens is achieved through various techniques, and the gradual posterior angulation of dens through aging and its transverse dimension should be considered with odontoid screw fixation technique [ 93]. Pediatric axis body and ring fracture including hangmanŌĆÖs fracture is rarely reported as a result of child abuse or high energy trauma [ 51, 84]. AxisŌĆÖs neurocentral or dens-arch synchondrosis should not be mistaken as fracture, but fracture through this synchondrosis is also reported. It is common to classify axis ring fracture by the system described by Effendi et al. [ 27] and modified by Levine and Edwards based on the degree of displacement and stability which provides clinically reasonable guideline for management. For type I or II fractures without neurologic deficit, conservative treatment with immobilization is generally sufficient for excellent bony union, but surgical treatment should be considered for LevineEdwards type IIa or III fractures with significant dislocation and possibility of later instability [ 17, 34, 60]. Axis body fractures are uncommon and mostly stable, but burst fracture with associated vertebral artery injury should not be missed [ 26].
Subaxial cervical spine injuries
Subaxial spinal injury refers to fracture, dislocation, or ligamentous injury of C3 to C7. Most common mechanism of injury is motor vehicle accidents, followed by sports injury and fall. Subaxial cervical spine injury mostly occurs between age 9 to 16 which reflects the fulcrum of cervical motion at C5-C6 for adolescents [ 9, 25]. For children under the age 9, pure ligamentous injury with SCI is more common, whereas bony injuries are more common for older children [ 65]. The most important determinant of treatment depends on neurologic status and stability of the injury, and imaging plays a key role for the evaluation [ 25, 70]. The decision whether to initiate cervical spine imaging for pediatric patients following blunt trauma can be aided by National Emergency X-Radiography Utilization Study tandard criteria [ 40, 99], bearing in mind that only 2.8% of the most difficult-to-assess group of age under 2 are included in the study [ 16], and that the usefulness of this criteria for pediatric population is being debated [ 28, 90]. Static plain radiographs of antero-posterior and lateral views are generally used with the advantage of less radiation exposure to the patient. Plain film with dynamic flexion and extension views are used to investigate instability although it may be unsatisfactory initially due to the muscle spasm or the need for immediate immobilization. For children under the age 8, angulation greater than 7┬░ or subluxation greater than 4.5 mm is generally considered unstable [ 70], which is the modification of the criteria by White and colleagues suited for adult population [ 101]. Supine CT can provide little information regarding stability, but still useful for bony anatomy and surgical planning. MRI is superior in revealing soft tissue, ligamentous, disc, or spinal cord injury. DenisŌĆÖs three column model, originally developed for thoracolumbar injury [ 21], is also widely used to assess cervical spine stability [ 10, 16], and Subaxial Cervical Spine Injury Classification (SLIC) system encompass treatment strategy with prognosis [ 53, 79, 97, 98]. Generally, stable injuries are managed conservatively, and surgical intervention is considered for mechanically or neurologically unstable injuries with shortest construct as possible to avoid compromising spinal column growth [ 65]. Future cervical deformity would require surgical treatment based on the degree of malalignment, as cervical spine is in a dynamic relationship with whole spine which can influence global spinal balance [ 47, 58]. Those who have objective finding of myelopathy from trauma, with negative plain radiographs, CT, and MRI are classified as SCIWORA, although some argue that this diagnosis can be made with cord signal change on MRI [ 16, 52]. Most investigators advocate conservative treatment of cervical orthosis for up to 12 weeks followed by examining for late instability for SCIWORA [ 52, 53, 65]. And it is noteworthy that some consider the term SCIWORA a misnomer especially for adult population because they actually have baseline degenerative changes [ 88]. Instead, the terms SCI without CT evidence of trauma (SCIWOCTET) or SCI without radiographic evidence of trauma (SCIWORET) are being advocated and used in literature as much as the traditional term, SCIWORA.
PEDIATRIC THORACOLUMBAR SPINE TRAUMA
Majority of pediatric thoracolumbar spine injury occur during adolescence age with male predominance, mostly by sport activities or motor vehicle accidents [ 14, 24]. Among all injury mechanisms, unrestrained motor vehicle accident is the culprit for more than half of SCI for all pediatric age groups [ 11, 100]. Injury types can be subdivided into compression fracture, burst fracture, fatigue fracture of pars interarticularis, seat belt fracture, slipped vertebral apophysis, shear injury, crushing injury, and SCIWORA. Stability of the spine and neurologic deficit are the most important part of assessment. Even mechanically stable injury can elicit neurologic deficit which warrants decompression or fusion operation. Specifically, shear injury is a form of fracture-dislocation type injury with instability at all three columns, and it should be kept in mind that burst fracture and slipped vertebral apophysis can damage germinative layer and lead to premature epiphyseal fusion. AOSpine thoracolumbar spine injury classification, DenisŌĆÖs three column model and thoracolumbar injury classification and severity score (TLICS) are all widely used for classification and treatment decision for pediatric population [ 3, 18, 19, 87]. Neurologically and mechanically stable thoracolumbar injuries can be treated conservatively with immobilization via orthosis. Besides, most neurologically intact burst fractures and potentially unstable injuries can also be treated nonoperatively with orthosis and bed rest [ 91]. The prognosis of SCIWORA depends on initial neurologic presentation and are usually treated conservatively [ 56, 91]. And it should be noted that children with further growth potential can develop chronic instability and subsequent deformity from spinal injuries, which may require surgery [ 20, 55]. In such cases, intuition from previous experience and research can be helpful. For spinal deformity surgery, global and regional alignment are important considerations for surgical planning [ 47- 49, 58]. Detailed decision including surgical approach, deformity correction technique, upper/lowest instrumented level, and adjunct material to use all matters and impacts clinicoradiological outcome [ 12, 41- 43, 78, 102].
CONCLUSION
Pediatric spine trauma patients require particular attention due to its unique anatomy and biomechanics. Treatment decision should be individualized with the insight based on previous investigations and physicianŌĆÖs thorough clinicoradiological assessment.
Fig.┬Ā1.
Spine computed tomography (CT) scan images of 6-year-old boy with lipomeningomyelocele and kyphosis. Neurocentral junction at T8 spine is noticeable from axial CT (arrows). 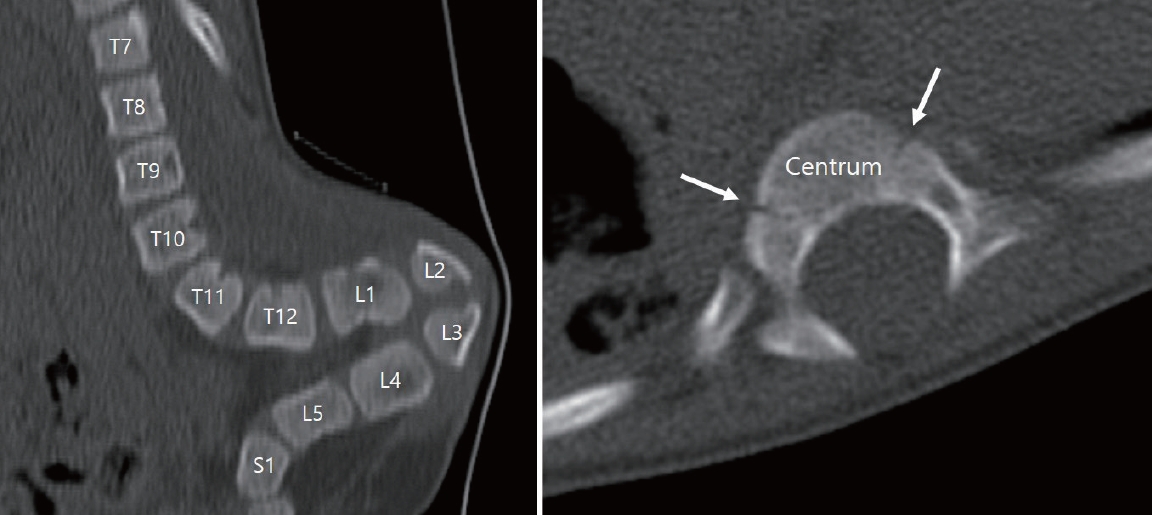
References
1. Abumi K, Fujiya M, Saita M, Kaneda K : Occipitoatlantal instability associated with articular tropism. Eur Spine J 7 : 76-79, 1998    2. Adams VI : Neck injuries: III. Ligamentous injuries of the craniocervical articulation without occipito-atlantal or atlanto-axial facet dislocation. A pathologic study of 21 traffic fatalities. J Forensic Sci 38 : 1097-1104, 1993   3. An Z, Zhu Y, Wang G, Wei H, Dong L : Is the thoracolumbar AOSpine injury score superior to the thoracolumbar injury classification and severity score for guiding the treatment strategy of thoracolumbar spine injuries? World Neurosurg 137 : e493-e498, 2020   4. Anderson PA, Montesano PX : Morphology and treatment of occipital condyle fractures. Spine (Phila Pa 1976) 13 : 731-736, 1988   5. Barber I, Perez-Rossello JM, Wilson CR, Silvera MV, Kleinman PK : Prevalence and relevance of pediatric spinal fractures in suspected child abuse. Pediatr Radiol 43 : 1507-1515, 2013   6. Baumann F, Ernstberger T, Neumann C, Nerlich M, Schroeder GD, Vaccaro AR, et al : Pediatric cervical spine injuries: a rare but challenging entity. J Spinal Disord Tech 28 : E377-E384, 2015  7. Been HD, Kerkhoffs GM, Maas M : Suspected atlantoaxial rotatory fixation-subluxation: the value of multidetector computed tomography scanning under general anesthesia. Spine (Phila Pa 1976) 32 : E163-E167, 2007  8. Bhatnagar M, Sponseller PD, Carroll C 4th, Tolo VT : Pediatric atlantoaxial instability presenting as cerebral and cerebellar infarcts. J Pediatr Orthop 11 : 103-107, 1991   9. Bonadio WA : Cervical spine trauma in children: part I. General concepts, normal anatomy, radiographic evaluation. Am J Emerg Med 11 : 158-165, 1993   10. Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, Papadopoulos SM, et al : Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976) 30 : 915-922, 2005   11. Carreon LY, Glassman SD, Campbell MJ : Pediatric spine fractures: a review of 137 hospital admissions. J Spinal Disord Tech 17 : 477-482, 2004  12. Choi HY, Hyun SJ, Kim KJ, Jahng TA, Kim HJ : Radiographic and clinical outcomes following pedicle subtraction osteotomy : minimum 2-year follow-up data. J Korean Neurosurg Soc 63 : 99-107, 2020   13. Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN : Spinal injuries in children. J Pediatr Surg 39 : 607-612, 2004   14. Clark P, Letts M : Trauma to the thoracic and lumbar spine in the adolescent. Can J Surg 44 : 337-345, 2001   15. Clayman DA, Sykes CH, Vines FS : Occipital condyle fractures: clinical presentation and radiologic detection. AJNR Am J Neuroradiol 15 : 1309-1315, 1994   16. Copley PC, Tilliridou V, Kirby A, Jones J, Kandasamy J : Management of cervical spine trauma in children. Eur J Trauma Emerg Surg 45 : 777-789, 2019   17. Coric D, Wilson JA, Kelly DL Jr : Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg 85 : 550-554, 1996   18. Dauleac C, Mottolese C, Beuriat PA, Szathmari A, Di Rocco F : Superiority of thoracolumbar injury classification and severity score (TLICS) over AOSpine thoracolumbar spine injury classification for the surgical management decision of traumatic spine injury in the pediatric population. Eur Spine J 30 : 3036-3042, 2021   19. Dawkins RL, Miller JH, Menacho ST, Ramadan OI, Lysek MC, Kuhn EN, et al : Thoracolumbar injury classification and severity score in children: a validity study. Neurosurgery 84 : E362-E367, 2019   20. Dearolf WW 3rd, Betz RR, Vogel LC, Levin J, Clancy M, Steel HH : Scoliosis in pediatric spinal cord-injured patients. J Pediatr Orthop 10 : 214-218, 1990   21. Denis F : The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 8 : 817-831, 1983   22. Desai SS, Coumas JM, Danylevich A, Hayes E, Dunn EJ : Fracture of the occipital condyle: case report and review of the literature. J Trauma 30 : 240-241, 1990  23. Dickman CA, Greene KA, Sonntag VK : Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery 38 : 44-50, 1996   24. Dogan S, Safavi-Abbasi S, Theodore N, Chang SW, Horn EM, Mariwalla NR, et al : Thoracolumbar and sacral spinal injuries in children and adolescents: a review of 89 cases. J Neurosurg 106( 6 Suppl):426-433, 2007   25. Dogan S, Safavi-Abbasi S, Theodore N, Horn E, Rekate HL, Sonntag VK : Pediatric subaxial cervical spine injuries: origins, management, and outcome in 51 patients. Neurosurg Focus 20 : E1, 2006  26. Durand D, Wu X, Kalra VB, Abbed KM, Malhotra A : Predictors of vertebral artery injury in isolated C2 fractures based on fracture morphology using CT angiography. Spine (Phila Pa 1976) 40 : E713-E718, 2015   27. Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA : Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br 63-B : 319-327, 1981   28. Ehrlich PF, Wee C, Drongowski R, Rana AR : Canadian C-spine rule and the national emergency X-radiography utilization low-risk criteria for C-spine radiography in young trauma patients. J Pediatr Surg 44 : 987-991, 2009   29. Fassett DR, McCall T, Brockmeyer DL : Odontoid synchondrosis fractures in children. Neurosurg Focus 20 : E7, 2006  30. Fesmire FM, Luten RC : The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med 7 : 133-142, 1989   31. Fielding JW, Hawkins RJ : Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am 59 : 37-44, 1977   32. Fujiwara H, Kaito T, Makino T, Yonenobu K : Positional occlusion of the vertebral artery in a case of rheumatoid atlantoaxial subluxation presenting with multiple cerebral and cerebellar infarction. Mod Rheumatol 22 : 605-609, 2012   33. Goel A : Torticollis and rotatory atlantoaxial dislocation: a clinical review. J Craniovertebr Junction Spine 10 : 77-87, 2019    34. Gornet ME, Kelly MP : Fractures of the axis: a review of pediatric, adult, and geriatric injuries. Curr Rev Musculoskelet Med 9 : 505-512, 2016    35. Hadley MN, Walters BC, Grabb PA, Oyesiku NM, Przybylski GJ, Resnick DK, et al : Diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 50( 3 Suppl):S105-S113, 2002   36. Hall GC, Kinsman MJ, Nazar RG, Hruska RT, Mansfield KJ, Boakye M, et al : Atlanto-occipital dislocation. World J Orthop 6 : 236-243, 2015    37. Harris JH Jr, Carson GC, Wagner LK : Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol 162 : 881-886, 1994   38. Harris JH Jr, Carson GC, Wagner LK, Kerr N : Radiologic diagnosis of traumatic occipitovertebral dissociation: 2. Comparison of three methods of detecting occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol 162 : 887-892, 1994   39. Herman MJ, Brown KO, Sponseller PD, Phillips JH, Petrucelli PM, Parikh DJ, et al : Pediatric cervical spine clearance: a consensus statement and algorithm from the Pediatric Cervical Spine Clearance Working Group. J Bone Joint Surg Am 101 : e1, 2019  40. Hoffman JR, Schriger DL, Mower W, Luo JS, Zucker M : Low-risk criteria for cervical-spine radiography in blunt trauma: a prospective study. Ann Emerg Med 21 : 1454-1460, 1992   41. Hyun SJ, Lenke LG, Kim Y, Bridwell KH, Cerpa M, Blanke KM : Adolescent idiopathic scoliosis treated by posterior spinal segmental instrumented fusion : when is fusion to L3 stable? J Korean Neurosurg Soc 64 : 776-783, 2021    42. Hyun SJ, Lenke LG, Kim Y, Bridwell KH, Cerpa M, Blanke KM : The incidence of adding-on or distal junctional kyphosis in adolescent idiopathic scoliosis treated by anterior spinal fusion to l3 was significantly higher than by posterior spinal fusion to L3. Neurospine 18 : 457-463, 2021    43. Hyun SJ, Yoon SH, Kim JH, Oh JK, Lee CH, Shin JJ, et al : A prospective, multi-center, double-blind, randomized study to evaluate the efficacy and safety of the synthetic bone graft material DBM gel with rhBMP-2 versus DBM gel used during the TLIF procedure in patients with lumbar disc disease. J Korean Neurosurg Soc 64 : 562-574, 2021    44. Jabbour P, Fehlings M, Vaccaro AR, Harrop JS : Traumatic spine injuries in the geriatric population. Neurosurg Focus 25 : E16, 2008  45. Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O'Connor KC, et al : Traumatic spinal cord injury in the United States, 1993-2012. JAMA 313 : 2236-2243, 2015    46. Judd DB, Liem LK, Petermann G : Pediatric atlas fracture: a case of fracture through a synchondrosis and review of the literature. Neurosurgery 46 : 991-994; discussion 994-995, 2000   47. Kim CW, Hyun SJ, Kim KJ : Surgical impact on global sagittal alignment and health-related quality of life following cervical kyphosis correction surgery: systematic review. Neurospine 17 : 497-504, 2020    48. Kim CW, Hyun SJ, Kim KJ : Systematic review of reciprocal changes after spinal reconstruction surgery : do not miss the forest for the trees. J Korean Neurosurg Soc 64 : 843-852, 2021    49. Kim DH, Hyun SJ, Kim KJ : Selection of fusion level for adolescent idiopathic scoliosis surgery : selective fusion versus postoperative decompensation. J Korean Neurosurg Soc 64 : 473-485, 2021    50. Kim YJ, Yoo CJ, Park CW, Lee SG, Son S, Kim WK : Traumatic atlantooccipital dislocation (AOD). Korean J Spine 9 : 85-91, 2012    51. Kleinman PK : Hangman's fracture caused by suspected child abuse. J Pediatr Orthop B 13 : 348author reply 348, 2004   52. Klimo P Jr, Ware ML, Gupta N, Brockmeyer D : Cervical spine trauma in the pediatric patient. Neurosurg Clin N Am 18 : 599-620, 2007   53. Konovalov N, Peev N, Zileli M, Sharif S, Kaprovoy S, Timonin S : Pediatric cervical spine injuries and SCIWORA: WFNS Spine Committee recommendations. Neurospine 17 : 797-808, 2020    54. Korean Statistical Information Service (KOSIS) : 2017 National children abuse report. Daejeon : KOSIS, 2017
55. Kulshrestha R, Kuiper JH, Masri WE, Chowdhury JR, Kaur S, Kumar N, et al : Scoliosis in paediatric onset spinal cord injuries. Spinal Cord 58 : 711-715, 2020   56. Launay F, Leet AI, Sponseller PD : Pediatric spinal cord injury without radiographic abnormality: a meta-analysis. Clin Orthop Relat Res 433 : 166-170, 2005
57. Lee C, Woodring JH, Goldstein SJ, Daniel TL, Young AB, Tibbs PA : Evaluation of traumatic atlantooccipital dislocations. AJNR Am J Neuroradiol 8 : 19-26, 1987   58. Lee SH, Hyun SJ, Jain A : Cervical sagittal alignment: literature review and future directions. Neurospine 17 : 478-496, 2020    59. Leventhal HR : Birth injuries of the spinal cord. J Pediatr 56 : 447-453, 1960   60. Li XF, Dai LY, Lu H, Chen XD : A systematic review of the management of hangman's fractures. Eur Spine J 15 : 257-269, 2006   61. Liao S, Jung MK, H├Črnig L, Gr├╝tzner PA, Kreinest M : Injuries of the upper cervical spine-how can instability be identified? Int Orthop 44 : 1239-1253, 2020   62. Lipson SJ : Rheumatoid arthritis in the cervical spine. Clin Orthop Relat Res 239 : 121-127, 1989  63. Ma F, He H, Liao Y, Tang Q, Tang C, Yang S, et al : Classification of the facets of lateral atlantoaxial joints in patients with congenital atlantoaxial dislocation. Eur Spine J 29 : 2769-2777, 2020   64. Maat GJ, Matricali B, van Persijn van Meerten EL : Postnatal development and structure of the neurocentral junction. Its relevance for spinal surgery. Spine (Phila Pa 1976) 21 : 661-666, 1996  65. Madura CJ, Johnston JM Jr : Classification and management of pediatric subaxial cervical spine injuries. Neurosurg Clin N Am 28 : 91-102, 2017   66. Mahr D, Freigang V, Bhayana H, Kerschbaum M, Frankewycz B, Loibl M, et al : Comprehensive treatment algorithm for atlanto-axial rotatory fixation (AARF) in children. Eur J Trauma Emerg Surg 47 : 713-718, 2021   67. Maiman DJ, Cusick JF : Traumatic atlantoaxial dislocation. Surg Neurol 18 : 388-392, 1982   68. Mandabach M, Ruge JR, Hahn YS, McLone DG : Pediatric axis fractures: early halo immobilization, management and outcome. Pediatr Neurosurg 19 : 225-232, 1993   69. Martinez-Lage JF, Martinez Perez M, Fernandez Cornejo V, Poza M : Atlanto-axial rotatory subluxation in children: early management. Acta Neurochir (Wien) 143 : 1223-1228, 2001   70. McCall T, Fassett D, Brockmeyer D : Cervical spine trauma in children: a review. Neurosurg Focus 20 : E5, 2006  71. Momjian S, Dehdashti AR, Kehrli P, May D, Rilliet B : Occipital condyle fractures in children. Case report and review of the literature. Pediatr Neurosurg 38 : 265-270, 2003    72. M├Čnckeberg JE, Tom├® CV, Mat├Łas A, Alonso A, V├Īsquez J, Zubieta JL : CT scan study of atlantoaxial rotatory mobility in asymptomatic adult subjects: a basis for better understanding C1-C2 rotatory fixation and subluxation. Spine (Phila Pa 1976) 34 : 1292-1295, 2009   73. Neal KM, Mohamed AS : Atlantoaxial rotatory subluxation in children. J Am Acad Orthop Surg 23 : 382-392, 2015   74. Pang D, Li V : Atlantoaxial rotatory fixation: part 1--biomechanics of normal rotation at the atlantoaxial joint in children. Neurosurgery 55 : 614-625; discussion 625-626, 2004   75. Pang D, Li V : Atlantoaxial rotatory fixation: part 2--new diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging. Neurosurgery 57 : 941-953; discussion 941-953, 2005   76. Pang D, Li V : Atlantoaxial rotatory fixation: part 3-a prospective study of the clinical manifestation, diagnosis, management, and outcome of children with alantoaxial rotatory fixation. Neurosurgery 57 : 954-972; discussion 954-972, 2005   77. Panjabi M, Dvorak J, Duranceau J, Yamamoto I, Gerber M, Rauschning W, et al : Three-dimensional movements of the upper cervical spine. Spine (Phila Pa 1976) 13 : 726-730, 1988   78. Park BJ, Hyun SJ, Wui SH, Jung JM, Kim KJ, Jahng TA : Surgical outcomes and complications following all posterior approach for spinal deformity associated with neurofibromatosis type-1. J Korean Neurosurg Soc 63 : 738-746, 2020    79. Patel AA, Hurlbert RJ, Bono CM, Bessey JT, Yang N, Vaccaro AR : Classification and surgical decision making in acute subaxial cervical spine trauma. Spine (Phila Pa 1976) 35( 21 Suppl):S228-S234, 2010   80. Pham MH, Cerpa M, Makhni MC, Sielatycki JA, Lenke LG : Neurologic deficit during halo-gravity traction in the treatment of severe thoracic kyphoscoliotic spinal deformity. Neurospine 17 : 461-465, 2020    81. Platzer P, Jaindl M, Thalhammer G, Dittrich S, Kutscha-Lissberg F, Vecsei V, et al : Cervical spine injuries in pediatric patients. J Trauma 62 : 389-396; discussion 394-39, 2007   82. Powers B, Miller MD, Kramer RS, Martinez S, Gehweiler JA Jr : Traumatic anterior atlanto-occipital dislocation. Neurosurgery 4 : 12-17, 1979   83. Radcliff KE, Hussain MM, Moldavsky M, Klocke N, Vaccaro AR, Albert TJ, et al : In vitro biomechanics of the craniocervical junction-a sequential sectioning of its stabilizing structures. Spine J 15 : 1618-1628, 2015   84. Ranjith RK, Mullett JH, Burke TE : Hangman's fracture caused by suspected child abuse. A case report. J Pediatr Orthop B 11 : 329-332, 2002   85. Rozzelle CJ, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Ryken TC, et al : Management of pediatric cervical spine and spinal cord injuries. Neurosurgery 72 Suppl 2 : 205-226, 2013  86. Salunke P, Sahoo SK, Deepak AN, Garg R : Congenital C1-2 lateral translational dislocation: case illustration with pre- and postoperative imaging. Pediatr Neurosurg 51 : 218-220, 2016   87. Savage JW, Moore TA, Arnold PM, Thakur N, Hsu WK, Patel AA, et al : The reliability and validity of the thoracolumbar injury classification system in pediatric spine trauma. Spine (Phila Pa 1976) 40 : E1014-E1018, 2015   88. Sayama C, Chen T, Trost G, Jea A : A review of pediatric lumbar spine trauma. Neurosurg Focus 37 : E6, 2014   89. Shim SC, Yoo DH, Lee JK, Koh HK, Lee SR, Oh SH, et al : Multiple cerebellar infarction due to vertebral artery obstruction and bulbar symptoms associated with vertical subluxation and atlanto-occipital subluxation in ankylosing spondylitis. J Rheumatol 25 : 2464-2468, 1998  90. Slaar A, Fockens MM, Wang J, Maas M, Wilson DJ, Goslings JC, et al : Triage tools for detecting cervical spine injury in pediatric trauma patients. Cochrane Database Syst Re 12 : CD011686, 2017  91. Slotkin JR, Lu Y, Wood KB : Thoracolumbar spinal trauma in children. Neurosurg Clin N Am 18 : 621-630, 2007   92. Stein DM, Knight WA 4th : Emergency neurological life support: traumatic spine injury. Neurocrit Care 27( Suppl 1):170-180, 2017   93. ┼Ātul├Łk J, Geri G, Salavcov├Ī L, Barna M, Fojt├Łk P, Na┼łka O : Pediatric dens anatomy and its implications for fracture treatment: an anatomical and radiological study. Eur Spine J 30 : 416-424, 2021   94. Theodore N, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, et al : The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 72 Suppl 2 : 114-126, 2013  95. Traynelis VC, Marano GD, Dunker RO, Kaufman HH : Traumatic atlantooccipital dislocation. Case report. J Neurosurg 65 : 863-870, 1986  96. Treloar DJ, Nypaver M : Angulation of the pediatric cervical spine with and without cervical collar. Pediatr Emerg Care 13 : 5-8, 1997   97. Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA Jr, et al : The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 32 : 2365-2374, 2007  98. Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, et al : AOSpine subaxial cervical spine injury classification system. Eur Spine J 25 : 2173-2184, 2016   99. Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR, et al : A prospective multicenter study of cervical spine injury in children. Pediatrics 108 : E20, 2001   100. Vitale MG, Goss JM, Matsumoto H, Roye DP Jr : Epidemiology of pediatric spinal cord injury in the United States: years 1997 and 2000. J Pediatr Orthop 26 : 745-749, 2006  101. White AA 3rd, Johnson RM, Panjabi MM, Southwick WO Jr : Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res 109 : 85-96, 1975  102. Wui SH, Hyun SJ, Kang B, Kim KJ, Jahng TA, Kim HJ : Bicortical screw purchase at upper instrumented vertebra (UIV) can cause UIV fracture after adult spinal deformity surgery: a finite element analysis study. Neurospine 17 : 377-383, 2020  
|
|