Lee, Park, Oh, Shin, and Park: Change in the Alignment and Distal Junctional Kyphosis Development after Posterior Cervical Spinal Fusion Surgery for Cervical Spondylotic Myelopathy - Risk Factor Analysis
Abstract
Objective
This study analyzed the risk factors in patients who developed distal junctional kyphosis (DJK) after posterior cervical fusion.
Methods
We retrospectively analyzed the clinical and radiographic outcomes of 64 patients, aged Ōēź18 years (51 and 13 male and female patients, respectively), who underwent single-staged multilevel (3-6 levels) posterior cervical fusion surgery due to multiple cervical spondylotic myelopathy. The surgeries were performed by a single spinal surgeon between January 2012 and December 2017. Demographic data, clinical outcomes, and radiological results were collected. We divided the patients into a DJK group and a non-DJK group according to the presence of DJK and investigated the risk factors by comparing the differences between the two groups.
Results
Of the 64 patients, 13 developed DJK. No significant differences in clinical results were observed between the two groups before and immediately after the surgery. At the final follow-up, a higher visual analog score for neck pain was observed in the DJK group compared to the non-DJK group (p<0.01). The DJK group had a significantly lower T1 slope and a significantly higher C2-7 sagittal vertical axis (SVA) before surgery compared to the non-DJK group (p=0.03 and p<0.01, respectively). Immediately after surgery, the difference between the two groups decreased and no significant difference was observed. However, at the last followup, a significantly higher C2-7 SVA was observed in the DJK group (p<0.01). At the last follow up, there is no discrepancy in T1S-CL. In multiple logistic regression analysis, preoperative higher C2-7 SVA and preoperative lower T1 slope were identified as independent risk factors (p=0.03 and p<0.01, respectively). As a result, it was confirmed that DJK occurred along the process of returning to preoperative values.
Conclusion
DJK can be considered to be caused by cervical misalignment due to excessive change in the surgical site in patients with low T1 slope and high C2-7 SVA before surgery. This also affects the clinical outcome after surgery. It is recommended to refrain from excessive segmental lordosis changes during multilevel cervical post fusion surgery, especially in patients with a small preoperative T1 slope and a large SVA value.
Key Words: Cervical vertebrae ┬Ę Spinal curvatures ┬Ę Radiology ┬Ę Pathology.
INTRODUCTION
Cervical spondylotic myelopathy (CSM) is one of the most common spinal disorders treated by spinal surgeons worldwide. CSM often presents in the elderly with several signs and symptoms, including neck pain, radiculopathy, or myelopathy [ 1, 28]. Posterior cervical spinal fusion with decompression is one of the possible treatment options in patients with CSM who have conditions such as spondylosis, spinal stenosis, and degenerative disc disease [ 24]. The development of distal junctional kyphosis (DJK) after cervical fusion surgery can be one of the possible concerns just like the development of proximal junctional kyphosis after thoracolumbar fusion surgery. DJK may lead to fixation failure, disc degeneration, distal level fractures, or spondylolisthesis, resulting in pain, myelopathy, or deformities [ 17]. The development of proximal junctional kyphosis and its characteristics and incidence following thoracolumbar fusion surgery have been well-known. However, the development of DJK following cervical spinal fusion surgery has not been studied or reported [ 4, 7, 18, 30]. In this study, the development and risk factors of DJK after posterior cervical spinal fusion surgery were analyzed.
MATERIALS AND METHODS
Study population
Approval for this study was obtained from the participating centerŌĆÖs Institutional Review Board of Gangneung Asan Hospital (IRB No. GNAH 2020-12-009). We retrospectively analyzed the clinical and radiographic outcomes of 64 patients aged Ōēź18 years (51 males and 13 females) who had multilevel CSM and underwent single-stage multilevel (3-6 levels) posterior cervical fusion surgery. The surgeries were performed by a single spine surgeon between January 2012 and December 2017. The surgical level was from C2 to C7. The Neck Disability Index (NDI) score and Visual analog score (VAS) of the arm and neck were used to measure clinical results. We also compared preoperative and postoperative (last follow-up) values.
Demographic data were collected for all patients, including age, sex, underlying disease, smoking history, body mass index (BMI), surgical details, follow-up information, electronic medical records, and radiographic image reviews. Exclusion criteria were previous cervical spine surgery, anterior surgery, follow-up less than 24 months, and surgery for other reasons.
We divided patients into DJK and non-DJK groups according to the presence of DJK at the last follow-up. DJK was defined as the changes of an angle of -10┬░ or less at the distal disc level from the end of the fusion construct between baseline and final follow up [ 23].
Surgical procedure
We performed cervical pedicle screw (CPS) insertion in all posterior cervical spinal fusion patients. The safety and efficacy of subaxial CPS placement have been validated multiple times [ 11, 20, 22]. Although the CPS placement with a freehand technique had been primarily considered, some lateral mass screw conversions or skipping of screw were also done [ 8, 31]. Following screw insertion and decompression, we extended the patientŌĆÖs head position using remote-controlled table head segments to achieve ideal lordosis from 15-30 degrees [ 1].
Radiologic evaluation
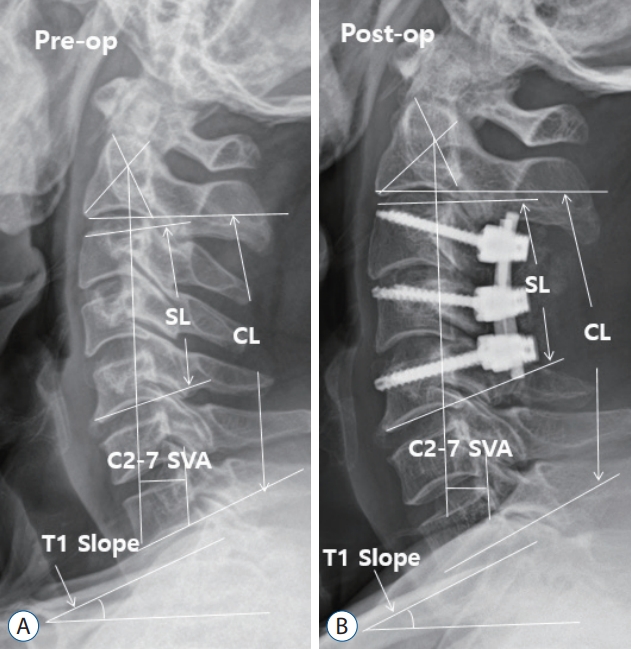
Cervical lordosis (CL) from C2 to C7, the T1 slope, the segmental angle index level, and the C2-7 sagittal vertical axis (SVA) were evaluated via lateral cervical X-ray ( Fig. 1). Radiographic parameters were measured before surgery, immediately after surgery, and at the last follow-up visit, and the changes in those parameters were analyzed. All radiographs were prepared using a photo archiving and communication system (PetaVision for Clinics version 2.0; Asan Medical Center, Seoul, Korea). All radiographic parameters were compared between the two groups.
Statistical analysis
Data are expressed as percentages and presented as mean┬▒ standard deviation. StudentŌĆÖs t-test was used to analyze the differences between continuous variables. p-values less than 0.05 were considered statistically significant, and multivariate logistic regression analysis was performed to identify independent factors that help predict the development of DJK after posterior cervical spinal fusion. Statistical Package for the Social Sciences (SPSS) Statistics for Windows, version 17.0 (IBM, Armonk, NY, USA), was used for all statistical analyses.
RESULTS
Demographic parameters
A total of 64 patients with multilevel CSM were included in this study, where 13 developed DJK and 51 did not. Of the 13 patients with DJK, three were asymptomatic and 10 experienced neck pain around the operated site (VAS score Ōēź4) after surgery ( Table 1). Only one among the 10 patients underwent revisional anterior cervical discectomy and fusion surgery to resolve radiculopathy caused by distal junctional problem. This patient, who underwent posterior C3-4-5-6 levels fusion surgery before 2 years, complained of radiculopathy caused by disc degeneration, stenosis, and kyphosis at C6-7 level. The mean patient age was 60.85┬▒10.18 years, and the mean follow-up period was 35.09┬▒11.13 months. No significant difference between DJK and non-DJK groups was observed in sex, age, underlying diseases, BMI, or smoking history ( Table 2).
Clinical outcomes
The clinical outcomes of all the patients showed improvement. There were no significant differences in the VAS scores of the arm or neck or in the NDI between the two groups before and after surgery. Higher NDI and VAS values were observed at the last follow-up in the DJK group than in the non-DJK group. A significant difference was observed in the VAS scores of the neck ( p=0.01) ( Table 3).
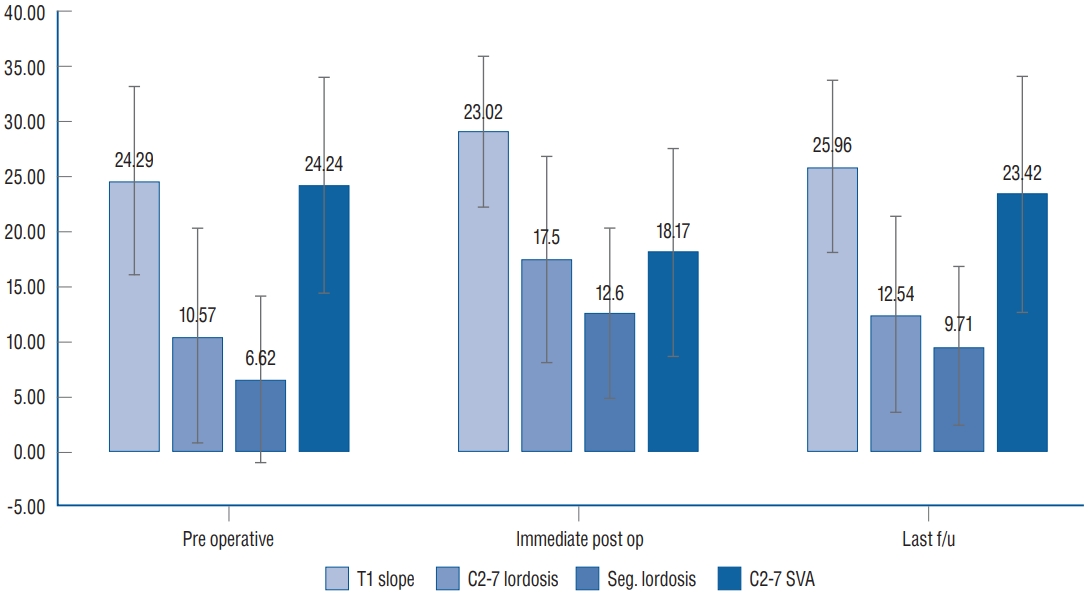
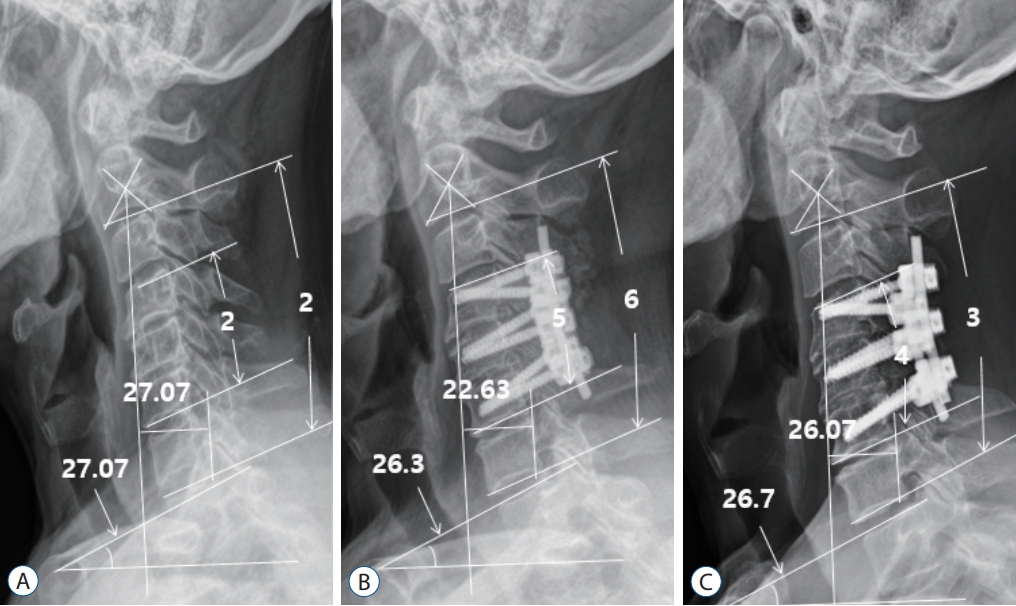
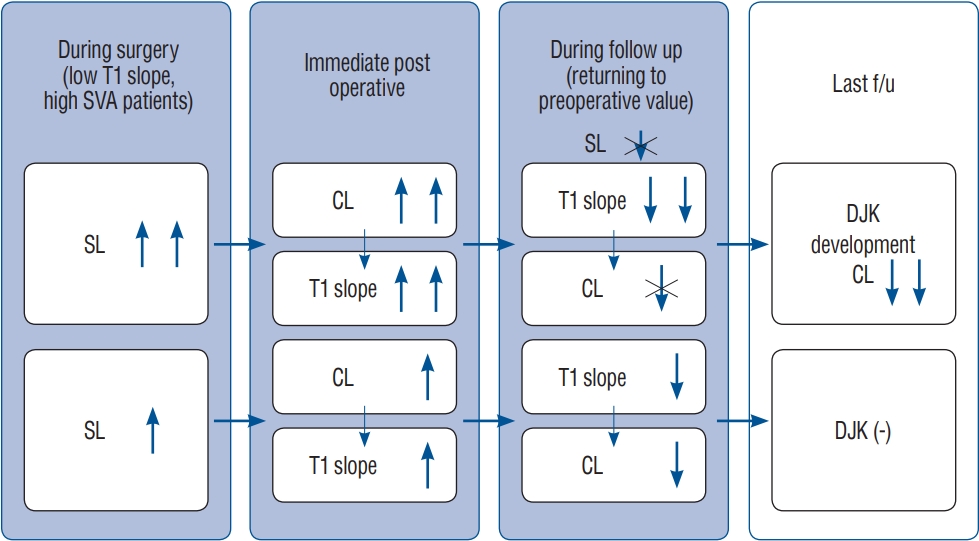
Radiographic outcomes
Significant differences were found in the T1 slope and C2-7 SVA ( p=0.03 and p<0.01; respectively) ( Table 4). Immediately after surgery, no significant difference in the T1 slope and C2-7 SVA was observed. However, at the last follow-up, a significant difference was observed in the C2-7 SVA (DJK group, 30.59┬▒13.88; non-DJK group, 21.57┬▒8.86; p<0.01). In all the patients, the cervical spinal radiological parameters tended to return to their preoperative values ( Figs. 2 and 3). When examining the changes between radiological parameters before surgery, immediately after surgery, and at the last follow-up, the changes in T1 slope, CL, and segmental angle before and immediately after surgery were significantly larger in the DJK group ( Table 5). The changes in CL, and T1-Cl mismatch between immediately after surgery and the last follow-up were significantly larger in the DJK group ( Table 6). Excessively lordotic segmental angle resulted in higher T1 slope, C2-7 SVA and CL changes in the immediately postoperative state. At the last follow-up, the T1 slope and C2-7 SVA return to the preoperative value, but the segmental lordosis (SL) did not return to the preoperative value. If the adjacent segment compensates for the alignment change of the index level appropriately, it becomes a non-DJK group, and if it is not compensated pathologically, DJK occurs ( Fig. 4). From the multiple logistic regression analysis of DJK occurrence, preoperative higher C2-7 SVA and preoperative lower T1 slope were identified as independent risk factors ( p=0.03 and p<0.01, respectively) ( Table 7).
DISCUSSION
We investigated the risk factors for DJK development after posterior decompression and fusion surgery. The T1 slope and CL displayed a tendency to return to their preoperative levels. Although many studies have been published on the relationship between the T1 slope and CL, to date [ 10, 14, 15], there is no previous report on the gradual alignment change after posterior cervical spinal fusion surgery resulting in DJK development. The return of the T1 slope and CL to preoperative levels may have resulted from patients tending to retain their preoperative spinopelvic alignments, which is due to the preservation of the preoperative T1 slope [ 2, 5]. This suggests that the T1 slope is the key parameter, with the CL depending on its value. Immediately after surgery, an increase in SL was associated with increases in the CL and T1 slope. During follow-up, because of the tendency to regain the preoperative T1 slope, the T1 slope decreased, followed by a decline in CL which inevitably related with DJK. Among the immediate postoperative parameters, only SL is amenable to surgical manipulation. The CL and T1 slope appeared to be dependent parameters following the SL changes. If greater SL changes are made during surgery, larger CL and T1 slope changes should also follow. However, the SL values did not return to preoperative levels despite gradual decreases after surgery. This observation may have been associated with the stiffness of the instrumentation ( Fig. 3). The multiple logistic regression analysis in this study showed that the preoperative C2-7 SVA and T1 slope are independent risk factors for DJK ( p<0.01 and p=0.03, respectively). In another study [ 23], preoperative cervical kyphosis (<-12┬░), preoperative cervical SVA (>56.3 mm), and preoperative CL-T1 slope (>36.4┬░) were analyzed as DJK risk predictors. It was also noted that patients with misalignment exceeding these thresholds had a 5-6 fold increased risk of DJK due to increased shear stress in the distal structures as cervical kyphosis increases the slope of the transition segment. These findings are similar to those in the lumbar deformity literature on the incidence of proximal junction kyphosis. Kim and Iyer [ 13] showed that in SVA, thoracic kyphosis, lumbar lordosis, sacral inclination, and pelvic retraction, poorer preoperative measures were found in the proximal junctional kyphosis. It has been described as leading to kyphosis. Neither age, sex, BMI, underlying disease, nor smoking significantly increased the risk of DJK. Although many studies have mentioned the relationship between smoking and cervical disc degeneration [ 16, 26], our result didnŌĆÖt show any significance. We found in this study that four of the 28 patients (14%) completed the post-fusion surgery at C6 and nine of the 31 patients (29%) ended up at C7. It has been found that DJK occurs at the cervicothoracic junction ( Table 1). Several studies [ 21, 25] have recommended cervicothoracic junction crossing fusion surgery to reduce the revision surgery rate due to adjustment segment disease in posterior fusion surgery involving the cervicothoracic junction. However, Truumees et al. [ 29] recommend it only for smokers or patients at high risk of pseudoarthrosis and to avoid in medically frail patients. Also, Kennamer et al. [ 9] mentioned that there is no particular difference in the revision rate as a result. Even in long instrumented spinal fusion surgery of the thoracolumbar spine, some studies recommend extension of the uppermost instrumented vertebrae to the upper thoracic level or at least above T10 to avoid proximal junctional kyphosis [ 19, 27]. However, other studies have reported that the risk of proximal junctional kyphosis was not increased with uppermost instrumented vertebrae at the thoracolumbar junction level compared to uppermost instrumented vertebrae above the thoracolumbar junction level [ 3, 6, 12]. Consequently, extension of the fusion to the thoracic level for DJK prevention remains controversial. In 2018, Passias et al. [ 23] found that the presence of neurological symptoms was the most appropriate predictor of DJK. In our study, there was no difference between the two groups immediately after surgery in terms of clinical outcomes, but worse results were observed in the DJK group in the VAS neck score at the last follow-up. There are some limitations to this study. First, this was a retrospective study. Second, the patients were examined only with X-ray imaging and not with computed tomography or magnetic resonance imaging. Finally, these results were derived from a small sample of patients. Studies with larger cohorts are needed. In addition, many patients who showed improvement were excluded because they did not meet the follow-up requirement, which may have resulted in selection bias.
CONCLUSION
In our study, risk factors of DJK in patients who developed DJK after posterior cervical fusion were analyzed. In patients with lower T1 slope and large C2-7 SVA, misalignment occurred due to excessive segment angle change during surgery, eventually resulting in DJK at last follow-up. In the clinical results, it was confirmed that the clinical results deteriorated again in the DJK group at the last follow-up. It is recommended to refrain from excessive SL changes during multilevel cervical post fusion surgery, especially in patients with a small preoperative T1 slope and a large SVA value.
Fig.┬Ā1.
Standard lateral cervical X-ray before and immediately after surgery. Standard lateral cervical X-ray before (A) and immediately after surgery (B). Pre-op : preoperative, SL : segmental lordosis, CL : cervical lordosis, SVA : sagittal vertical axis, Post-op : postoperative. 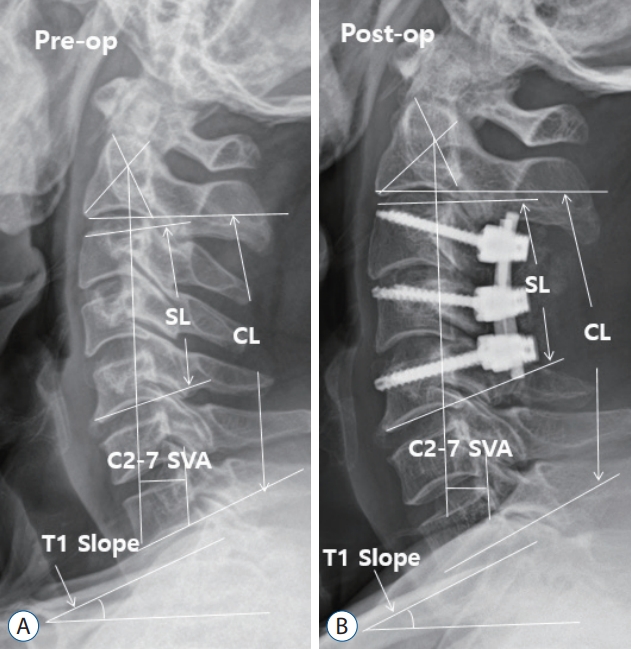
Fig.┬Ā2.
T1 slope, cervical lordosis, segmental lordosis and sagittal vertical axis values preoperatively, postoperatively, and at the final follow-up. Final follow-up and preoperative values for T1 slope, cervical lordosis, and sagittal vertical axis were similar. These similarities were statistically significant (p<0.01). op : operation, f/u : follow-up, Seg. : segmental, SVA : sagittal vertical axis. 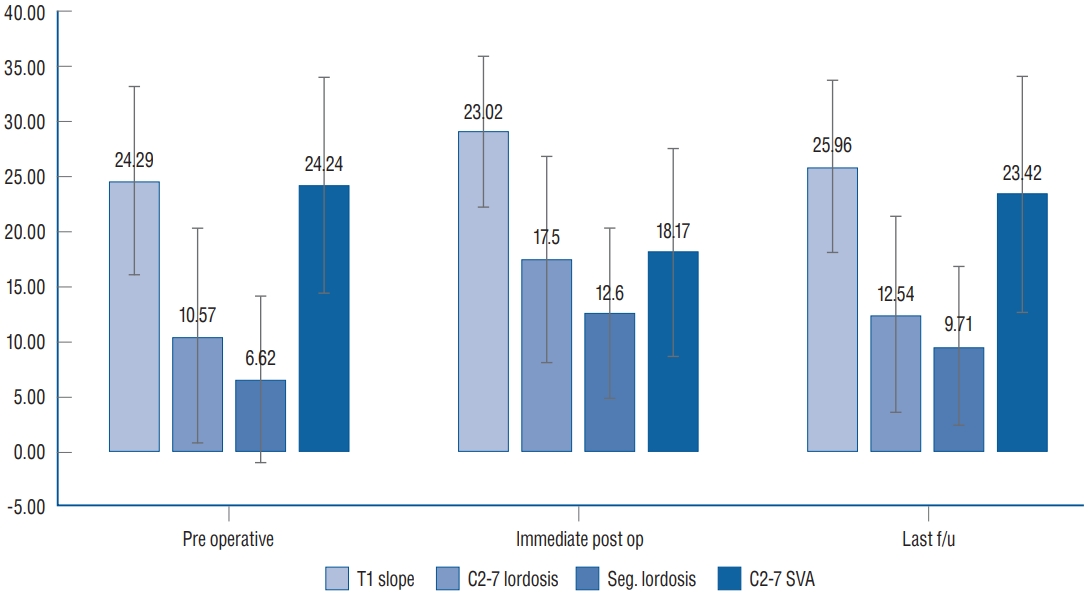
Fig.┬Ā3.
CL, SL, T1 slope increased and C2-7 SVA decreased immediately but eventually returned to preoperative values (A). Changes to T1 slope, CL, SL, and C2-7 SVA immediately postoperatively (B) and at the final follow-up (C). CL : cervical lordosis, SL : segmental lordosis, SVA : sagittal vertical axis. 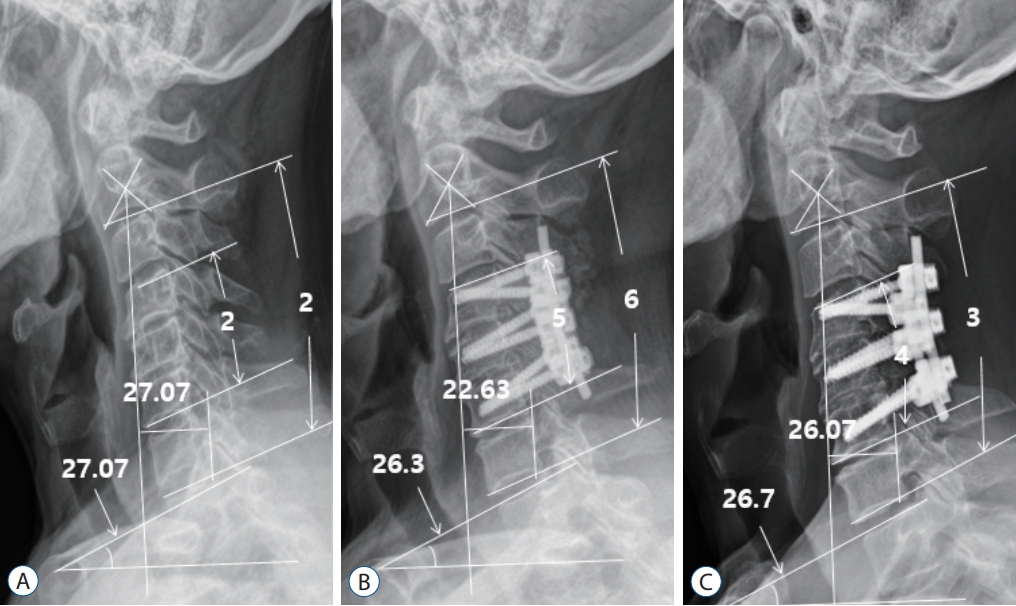
Fig.┬Ā4.
Algorithm of DJK development. SVA : sagittal vertical axis, SL : segmental lordosis, CL : cervical lordosis, f/u : follow-up, DJK : distal junctional kyphosis. 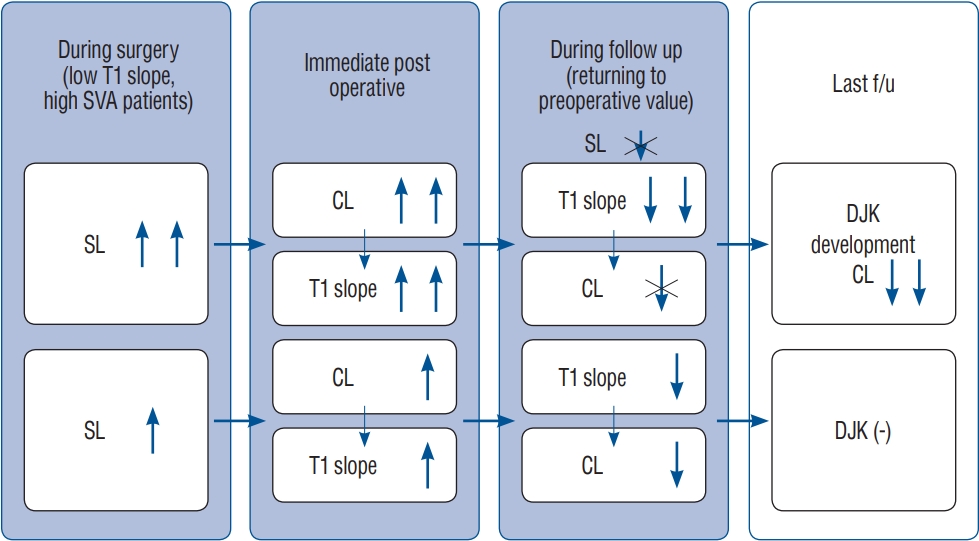
Table┬Ā1.
Characteristics of patients who developed DJK after surgery
|
No. |
Age (years)/sex |
Fusion level |
Follow-up duration (months) |
Revision |
Symptom at last follow-up |
|
1 |
55/M |
C3-4-5-6-7 |
27 |
X |
Posterior neck pain |
|
2 |
70/F |
C4-5-6-7 |
23 |
X |
Asymptomatic |
|
3 |
76/M |
C3-4-5-6-7 |
24 |
X |
Posterior neck pain |
|
4 |
64/M |
C3-4-5-6-7 |
30 |
X |
Posterior neck pain |
|
5 |
55/M |
C3-4-5-6 |
38 |
X |
Posterior neck pain |
|
6 |
63/F |
C3-4-5-6 |
24 |
X |
Posterior neck pain |
|
7 |
47/M |
C4-5-6-7 |
24 |
X |
Posterior neck pain |
|
8 |
80/F |
C4-5-6 |
30 |
X |
Asymptomatic |
|
9 |
55/M |
C5-6-7 |
32 |
X |
Posterior neck pain |
|
10 |
73/M |
C3-4-5-6 |
36 |
ACDF C6-7 |
Posterior neck pain and radiculopathy |
|
11 |
57/M |
C5-6-7 |
26 |
X |
Posterior neck pain |
|
12 |
69/M |
C4-5-6-7 |
25 |
X |
Asymptomatic |
|
13 |
55/M |
C3-4-5-6-7 |
24 |
X |
Posterior neck pain |
Table┬Ā2.
Demographics of the DJK and non-DJK groups
|
DJK group (n=13) |
Non-DJK group (n=51) |
p-value |
|
Age (years) |
62.15┬▒9.50 |
60.52┬▒10.41 |
0.61 |
|
Sex, M : F |
8 : 5 |
45 : 6 |
0.28 |
|
Fusion level |
3.30┬▒0.85 |
2.84┬▒0.88 |
0.09 |
|
Hypertension |
6 |
17 |
0.39 |
|
Diabetes mellitus |
4 |
11 |
0.43 |
|
Smoking |
6 |
19 |
0.19 |
|
Body mass index (kg/m2) |
24.19┬▒2.66 |
24.47┬▒3.56 |
0.79 |
|
Follow-up duration (months) |
39.31┬▒12.44 |
28.83┬▒12.14 |
0.14 |
Table┬Ā3.
Clinical outcomes for each period in both groups
|
DJK group (n=13) |
Non-DJK group (n=51) |
p-value |
|
VAS, neck |
|
|
|
|
ŌĆāPreoperative |
7.69┬▒1.31 |
7.11┬▒2.02 |
0.33 |
|
ŌĆāPostoperative |
2.23┬▒1.96 |
3.41┬▒2.25 |
0.08 |
|
ŌĆāLast f/u |
2.63┬▒1.75 |
1.62┬▒1.19 |
0.01 |
|
VAS, arm |
|
|
|
|
ŌĆāPreoperative |
5.53┬▒2.75 |
6.72┬▒2.20 |
0.10 |
|
ŌĆāPostoperative |
1.92┬▒0.86 |
2.76┬▒1.64 |
0.09 |
|
ŌĆāLast f/u |
2.61┬▒1.60 |
2.31┬▒1.71 |
0.56 |
|
NDI |
|
|
|
|
ŌĆāPreoperative |
26.76┬▒11.05 |
26.50┬▒10.77 |
0.93 |
|
ŌĆāPostoperative |
10.07┬▒7.34 |
13.43┬▒9.51 |
0.24 |
|
ŌĆāLast f/u |
15.61┬▒8.37 |
10.47┬▒8.45 |
0.06 |
Table┬Ā4.
Comparison of radiologic parameters between the DJK and non-DJK groups
|
DJK group (n=13) |
Non-DJK group (n=51) |
p-value |
|
T1 slope (┬░) |
|
|
|
|
ŌĆāPreoperative |
20.26┬▒6.53 |
25.64┬▒8.57 |
0.03 |
|
ŌĆāImmediate postoperative |
28.94┬▒7.53 |
29.03┬▒6.67 |
0.96 |
|
ŌĆāLast f/u |
24.20┬▒8.31 |
26.41┬▒8.31 |
0.36 |
|
CL (┬░) |
|
|
|
|
ŌĆāPreoperative |
8.07┬▒9.07 |
11.21┬▒9.07 |
0.29 |
|
ŌĆāImmediate postoperative |
19.38┬▒11.27 |
17.01┬▒8.62 |
0.41 |
|
ŌĆāLast f/u |
9.84┬▒9.71 |
13.23┬▒8.63 |
0.22 |
|
SL (┬░) |
|
|
|
|
ŌĆāPreoperative |
4.69┬▒7.75 |
7.11┬▒7.57 |
0.30 |
|
ŌĆāImmediate postoperative |
15.15┬▒11.31 |
11.96┬▒6.40 |
0.18 |
|
ŌĆāLast f/u |
11.38┬▒10.68 |
9.58┬▒6.40 |
0.43 |
|
C2-7 SVA (mm) |
|
|
|
|
ŌĆāPreoperative |
31.92┬▒9.24 |
22.29┬▒8.95 |
<0.01 |
|
ŌĆāImmediate postoperative |
22.13┬▒8.54 |
16.96┬▒9.24 |
0.08 |
|
ŌĆāLast f/u |
30.59┬▒13.88 |
21.57┬▒8.86 |
<0.01 |
|
T1 slope - CL(┬░) |
|
|
|
|
ŌĆāPreoperative |
12.18┬▒4.40 |
14.42┬▒6.68 |
0.25 |
|
ŌĆāImmediate postoperative |
9.56┬▒6.45 |
12.02┬▒7.53 |
0.28 |
|
ŌĆāLast f/u |
16.63┬▒5.72 |
13.18┬▒7.79 |
0.14 |
Table┬Ā5.
Differences in cervical parameters before and after surgery
|
DJK group (n=16) |
Non-DJK group (n=25) |
p-value |
|
Δ T1 slope |
8.69┬▒4.04 |
3.40┬▒5.81 |
0.03 |
|
Δ CL |
11.30┬▒7.34 |
5.80┬▒7.25 |
0.01 |
|
Δ SL |
10.46┬▒7.95 |
4.84┬▒6.04 |
<0.01 |
|
Δ C2-7 SVA |
8.94┬▒5.32 |
5.34┬▒6.80 |
0.08 |
|
Δ T1 - CL |
2.61┬▒4.51 |
2.40┬▒6.82 |
0.91 |
Table┬Ā6.
Differences in cervical parameters immediately postoperatively and at the final follow-up
|
DJK group (n=16) |
Non-DJK group (n=25) |
p-value |
|
Δ T1 slope |
4.74┬▒3.11 |
2.62┬▒3.96 |
0.07 |
|
Δ CL |
9.53┬▒5.39 |
3.78┬▒4.77 |
<0.01 |
|
Δ SL |
3.76┬▒2.91 |
2.37┬▒2.51 |
0.08 |
|
ΔC2-7 SVA |
7.22┬▒8.18 |
4.74┬▒5.32 |
0.10 |
|
Δ T1 - CL |
7.06┬▒7.78 |
1.15┬▒4.60 |
<0.01 |
Table┬Ā7.
Multivariable stepwise logistic regression analysis results for factors influencing DJK after posterior cervical spinal fusion surgery
|
Risk factor |
OR |
95% CI |
p-value |
|
Preoperative T1 slope |
0.49 |
0.29-0.81 |
<0.01 |
|
Preoperative SVA |
1.42 |
1.13-1.78 |
0.03 |
References
1. Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, et al : Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 38( 22 Suppl 1):S149-S160, 2013  2. Cho JH, Ha JK, Kim DG, Song KY, Kim YT, Hwang CJ, et al : Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine (Phila Pa 1976) 39 : E1575-E1581, 2014   4. Daubs MD : Sagittal alignment changes and proximal junctional kyphosis in adolescent idiopathic scoliosis. Spine J 16 : 784-785, 2016   6. Ha Y, Maruo K, Racine L, Schairer WW, Hu SS, Deviren V, et al : Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 19 : 360-369, 2013   7. Inaparthy P, Queruz JC, Bhagawati D, Thakar C, Subramanian T, Nnadi C : Incidence of proximal junctional kyphosis with magnetic expansion control rods in early onset scoliosis. Eur Spine J 25 : 3308-3315, 2016    8. Karaikovic EE, Yingsakmongkol W, Gaines RW Jr : Accuracy of cervical pedicle screw placement using the funnel technique. Spine (Phila Pa 1976) 26 : 2456-2462, 2001   9. Kennamer BT, Arginteanu MS, Moore FM, Steinberger AA, Yao KC, Gologorsky Y : Complications of poor cervical alignment in patients undergoing posterior cervicothoracic laminectomy and fusion. World Neurosurg 122 : e408-e414, 2019   10. Kim B, Yoon DH, Ha Y, Yi S, Shin DA, Lee CK, et al : Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J 16 : 219-225, 2016   11. Kim HB, Lee MK, Lee YS, Sohn JY, Jung SK, Park JH : An assessment of the medial angle of inserted subaxial cervical pedicle screw during surgery: practical use of preoperative CT scanning and intraoperative Xrays. Neurol Med Chir (Tokyo) 57 : 159-165, 2017    12. Kim HJ, Boachie-Adjei O, Shaffrey CI, Schwab F, Lafage V, Bess S, et al : Upper thoracic versus lower thoracic upper instrumented vertebrae endpoints have similar outcomes and complications in adult scoliosis. Spine (Phila Pa 1976) 39 : E795-E759, 2014   13. Kim HJ, Iyer S : Proximal junctional kyphosis. J Am Acad Orthop Surg 24 : 318-326, 2016   14. Kim TH, Lee SY, Kim YC, Park MS, Kim SW : T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 38 : E992-E997, 2013   15. Knott PT, Mardjetko SM, Techy F : The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 10 : 994-998, 2010   16. Livshits G, Cohen Z, Higla O, Yakovenko K : Familial history, age and smoking are important risk factors for disc degeneration disease in arabic pedigrees. Eur J Epidemiol 17 : 643-651, 2001  17. Lowe TG, Lenke L, Betz R, Newton P, Clements D, Haher T, et al : Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: incidence, risk factors, and prevention. Spine (Phila Pa 1976) 31 : 299-302, 2006   18. McClendon J Jr, Smith TR, Sugrue PA, Thompson SE, OŌĆÖShaughnessy BA, Koski TR : Spinal implant density and postoperative lumbar lordosis as predictors for the development of proximal junctional kyphosis in adult spinal deformity. World Neurosurg 95 : 419-424, 2016   19. O'Shaughnessy BA, Bridwell KH, Lenke LG, Cho W, Baldus C, Chang MS, et al : Does a long-fusion ŌĆ£T3-sacrumŌĆØ portend a worse outcome than a short-fusion ŌĆ£T10-sacrumŌĆØ in primary surgery for adult scoliosis? Spine (Phila Pa 1976) 37 : 884-890, 2012   20. Oe S, Togawa D, Nakai K, Yamada T, Arima H, Banno T, et al : The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine (Phila Pa 1976) 40 : 1487-1494, 2015   21. Osterhoff G, Ryang YM, Von Oelhafen J, Meyer B, Ringel F : Posterior multilevel instrumentation of the lower cervical spine: is bridging the cervicothoracic junction necessary? World Neurosurg 103 : 419-423, 2017   22. Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC : The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine (Phila Pa 1976) 39 : 280-285, 2014  23. Passias PG, Vasquez-Montes D, Poorman GW, Protopsaltis T, Horn SR, Bortz CA, et al : Predictive model for distal junctional kyphosis after cervical deformity surgery. Spine J 18 : 2187-2194, 2018   24. Salzmann SN, Derman PB, Lampe LP, Kueper J, Pan TJ, Yang J, et al : Cervical spinal fusion: 16-year trends in epidemiology, indications, and in-hospital outcomes by surgical approach. World Neurosurg 113 : e280-e295, 2018   25. Schroeder GD, Kepler CK, Kurd MF, Mead L, Millhouse PW, Kumar P, et al : Is it necessary to extend a multilevel posterior cervical decompression and fusion to the upper thoracic Spine? Spine (Phila Pa 1976) 41 : 1845-1849, 2016   27. Shufflebarger H, Suk SI, Mardjetko S : Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine (Phila Pa 1976) 31( 19 Suppl):S185-S194, 2006  28. Smith JS, Lafage V, Ryan DJ, Shaffrey CI, Schwab FJ, Patel AA, et al : Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine (Phila Pa 1976) 38( 22 Suppl 1):S161-S170, 2013  29. Truumees E, Singh D, Geck MJ, Stokes JK : Should long-segment cervical fusions be routinely carried into the thoracic spine? A multicenter analysis. Spine J 18 : 782-787, 2018   30. Yan P, Bao H, Qiu Y, Bao M, Varghese JJ, Sun X, et al : Mismatch between proximal rod contouring and proximal junctional angle: a predisposed risk factor for proximal junctional kyphosis in degenerative scoliosis. Spine (Phila Pa 1976) 42 : E280-E287, 2017 
|
|