Sim, Park, Choi, and Kim: Demonstration of Traumatic Subarachnoid Hemorrhage from the Anterior Choroidal Artery
Abstract
We present a case of angiographically confirmed transection of the cisternal segment of the anterior choroidal artery (AChA) associated with a severe head trauma in a 15-year old boy. The initial brain computed tomography scan revealed a diffuse subarachnoid hemorrhage (SAH) and pneumocephalus with multiple skull fractures. Subsequent cerebral angiography clearly demonstrated a complete transection of the AChA at its origin with a massive extravasation of contrast medium as a jet trajectory creating a plume. We speculate that severe blunt traumatic force stretched and tore the left AChA between the internal carotid artery and the optic tract. In a simulation of the patient's brain using a fresh-frozen male cadaver, the AChA is shown to be vulnerable to stretching injury as the ipsilateral optic tract is retracted. We conclude that the arterial injury like an AChA rupture should be considered in the differential diagnosis of severe traumatic SAH.
Key Words: Traumatic subarachnoid hemorrhage В· Anterior choroidal artery В· Transection В· Angiography В· Cadaver.
INTRODUCTION
Traumatic subarachnoid hemorrhage (tSAH) is a common finding following acute brain injury 5). Often, cerebral angiography is not performed when tSAH is diagnosed on brain computed tomography (CT) because of the low frequency of an identifiable source of arterial bleeding and relatively good outcomes in cases of isolated tSAH following low force impact. While majority of tSAH is associated with rupture of the vertebral artery, fatal traumatic dissection of the internal carotid artery has been rarely reported in the literature 2,4,6,7,9,10). Furthermore, there is little consensus regarding the mechanism of the injury in tSAH. Here, we describe a case of tSAH due to transection of the cisternal segment of the AChA that is clearly demonstrated by angiography. The mechanism underlying cisternal AChA transection following trauma is believed to be related to the anatomical position of cisternal AChA and its two attachments to the internal carotid artery (ICA) and the optic tract respectively. Using a human cadaver and computer imaging, we reproduced the anatomic vulnerability to vascular injury at that site.
CASE REPORT
A previously healthy 15-year-old boy who was not wearing a seatbelt was severely injured after being thrown into the driver's seat when the bus he was riding in collided with another vehicle. Upon admission, the patient was in cardiopulmonary arrest with the pupils dilated and not reactive to light. Intensive resuscitative procedures produced a response; however, the patient remained in a deep coma. Externally, extensive scalp lacerations and intractable massive epistaxis were observed. A chest X-ray revealed a left tension pneumothorax.
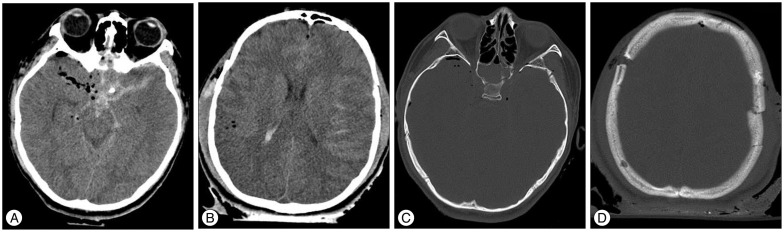
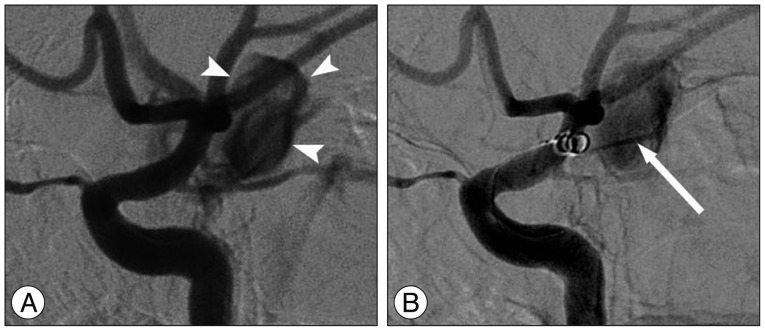
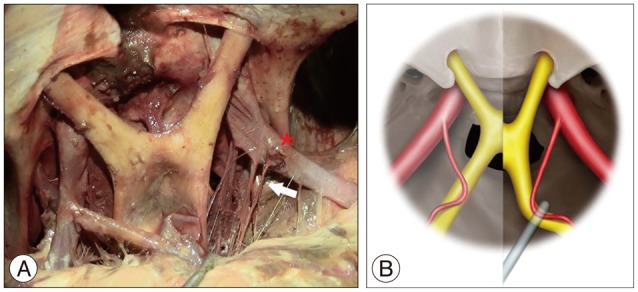
Brain CT revealed a thick, diffuse SAH with pneumocephalus at the base of the brain and in the cerebral convexities ( Fig. 1), as well as multiple skull fractures involving the sphenoid sinus and both temporoparietal bones, including the coronal suture, but no bone fragments were present in the basal cistern. Chest and abdomen CT showed a large pneumothorax in the left chest and moderate hemoperitoneum and a splenic laceration. Arteriography revealed active bleeding foci in the spleen, and the splenic artery was subsequently embolized with pushable coils. Cerebral angiography demonstrated active contrast medium extravasation with a jet trajectory creating a plume from the origin of the left AChA, without a visible aneurysm or any other vascular abnormalities ( Fig. 2). However, endovascular coil packing to control bleeding failed and the patient died 3 hours after the accident. We attempted a simulation of the patient's situation in the brain using a fresh-frozen male cadaver. The anterior cerebral arteries were removed to expose the AChAs and the optic tracts. As seen in the figure, the optico-carotid cisterns is widen and the AChA is stretched compared to normal due to the gravity effect of the patient head position and the retraction of the frontal lobes ( Fig. 3). Using the cadaver, we reproduced the possible injuries to the AChA during severe head trauma. In our simulation when the left optic tract was pulled tense, the AChA was particularly strained and stretched ( Fig. 3).
DISCUSSION
The majority of severe tSAH is associated with rupture of the vertebrobasilar arteries and dissection of the ICA is an exceedingly rare finding, reported in less than 0.2% of all head trauma 2,4,6,7,9,10). In 1959, Mosberg and Lindenberg 8) reported the first case of traumatic pallidal hemorrhage from the AChA with a definite pathological correlation at autopsy. They also reviewed 20 other autopsy cases with traumatic pallidal hemorrhage. Based on their findings, they postulated that the lesion-producing mechanism involved the intracerebral twigs of the AChA. Here, we report the first case of traumatic SAH due to transection of the cisternal segment of the AChA and show that contrast medium ex-travasation was clearly visible as a jet trajectory creating a plume during cerebral angiography ( Fig. 2). Anatomically, the cisternal segment of the AChA originates from the posterolateral wall of the ICA, runs along the lateral recess of the basal cistern, attaches itself to the optic tract, which is follows to reach the crural cistern before entering the choroidal fissure. The optic tracts are also attached to two different locations. Anteriorly, they are posterolateral extensions of the optic chiasm, which lies almost wholly over the diaphragma sellae. Posteriorly, the optic tracts are attached to the cerebrum and cerebral peduncles. Unlike the anterior aspect, which is firmly anchored to the optic canal through the optic nerve, the posterior aspect of the optic tract offers relatively little resistance to brain movement. Therefore, they can be retracted with brain movement due to severe blunt trauma.
There is little consensus regarding the mechanism of injury in tSAH. In our case, direct injury to the AChA by basal skull fracture and tearing by bony prominences was ruled out with brain CT findings. There was no bony fragment around the implicated area in the left optico-carotid cistern. The basal skull fracture, which was extended diagonally from the left temporal bone to the right side of the sphenoid sinus traversing the sellar turcica, was present in the contralateral side of the implicated lesion ( Fig. 1). So we speculate the mechanism of our case should be excessive stretch of AChA caused by vigorous movement of the brain. From a pathophysiologic viewpoint, a sharp blow to the head could result in displacement of the ICA against the optic tract, displacement of the optic tract against the ICA, or a combination of the two. This could stretch and tear the cisternal segment of the AChA, which is fixed between the two structures. Usually, the caliber of the AChA narrows as it travels, making the AChA vulnerable to strain injury. An autopsy study of an adult male revealed that the diameter beyond the optical tract was as small as 0.70Вұ0.16 mm (range : 0.6-0.98 mm) with a length of approximately 12 mm 1,3). Additionally, if the chiasm is displaced and/or distorted by a basilar skull fracture, the optic tract can shift and increase tension on the cisternal segment of the AChA. Most traumatic SAH following blunt trauma is self-limited. However, care must be taken to detect arterial injury like AChA rupture and fatal hemorrhage. Emergency catheter angiography is indicated if clinical signs or symptoms develop or progress rapidly or if CT shows ongoing hemorrhage or vascular injury. It is important to diagnose hemorrhage immediately and to plan definitive trans-catheter or surgical therapy. Treatments include endovascular therapy or surgical trapping with or without cerebral revascularization should be considered. Consideration for emergent cerebral angiography with embolization should be given for severe traumatic basal SAH. We attempted transcatheter embolization of the active hemorrhage from the point of AChA transection rather than an open surgical approach for several reasons : we desired rapid occlusion, surgical access was difficult, and the patient was a poor candidate for surgery. However, he expired 3 hours after the accident during an attempt to insert an endovascular stent after the failure of selective arterial coil embolization.
CONCLUSION
This is the first case of traumatic SAH due to transection of the cisternal segment of the AChA at its origin causing massive extravasation with a jet trajectory of the contrast medium during cerebral angiography. We demonstrated that the likely mechanism is a sharp blow to the head causing marked brain shift leading to stretching and eventual tearing of the AChA between the ICA and the neurovascular bundle.
Acknowledgements
The authors would like to thank Sangwon Yeo, medical illustrator, Dept. of Neurosurgery, University of Texas Health Science Center at Houston, for his help in preparing the artwork.
References
1. Baskaya MK, Coscarella E, Gomez F, Morcos JJ : Surgical and angiographic anatomy of the posterior communicating and anterior choroidal arteries. Neuroanatomy 2004, 3 : 38-42,
2. Bunai Y, Nagai A, Nakamura I, Ohya I : Traumatic rupture of the basilar artery : report of two cases and review of the literature. Am J Forensic Med Pathol 2000, 21 : 343-348,   3. ГҮakmak YГ–, Г–zdoДҹmuЕҹ Г–, GГјrdal E, Uzun Д°, ГҮavdar S : Origins and diameter of the anterior choroidal artery. Marmara Med J 2009, 22 : 123-126,
4. Filter ER, Fernandes JR : Fatal traumatic subarachnoid hemorrhage due to assault-related tear of the basilar artery. J Forensic Leg Med 2009, 16 : 414-416,   5. Fung C, Z'Graggen WJ, Beck J, Gralla J, Jakob SM, Schucht P, et al : Trau-matic subarachnoid hemorrhage, basal ganglia hematoma and ischemic stroke caused by a torn lenticulostriate artery. Acta Neurochir (Wien) 2012, 154 : 59-62,   6. Gross A : Traumatic basal subarachnoid hemorrhages : autopsy material analysis. Forensic Sci Int 1990, 45 : 53-61,   7. Harland WA, Pitts JF, Watson AA : Subarachnoid haemorrhage due to upper cervical trauma. J Clin Pathol 1983, 36 : 1335-1341,    8. Mosberg WH, Lindenberg R : Traumatic hemorrhage from the anterior choroidal artery. J Neurosurg 1959, 16 : 209-221,   9. Pollanen MS, Deck JH, Blenkinsop B : Injury of the tunica media in fatal rupture of the vertebral artery. Am J Forensic Med Pathol 1996, 17 : 197-201,   10. Simonsen J : Fatal subarachnoid haemorrhages in relation to minor injuries in Denmark from 1967 to 1981. Forensic Sci Int 1984, 24 : 57-63,  
Fig.В 1
Cranial CT scan at admission revealed severe tSAH in the basal cistern and pneumocephalus predominantly in the right Sylvian fissure (A and B) and an extensive basal skull fracture extending from the left temporal bone to the right side of the sphenoid sinus and sella turcica (C) and a diastatic fracture through the coronary suture and communicated fracture of the left parietal bone (D). CT : computed tomography, tSAH : traumatic subarachnoid hemorrhage. 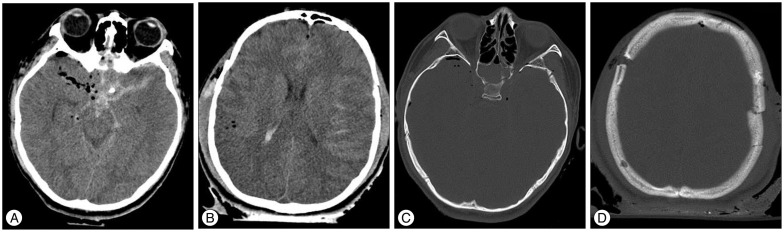
Fig.В 2
Digital subtraction cerebral angiography revealed massive contrast media extravasation from the ICA distal to posterior communicating artery (arrowheads) (A), and the extravasation from the origin of the AChA showed a jet trajectory of the contrast medium (arrow) (B). The coil passing through the AChA origin did not prevent the leaking of the contrast media. ICA : internal carotid artery, AChA : anterior choroidal artery. 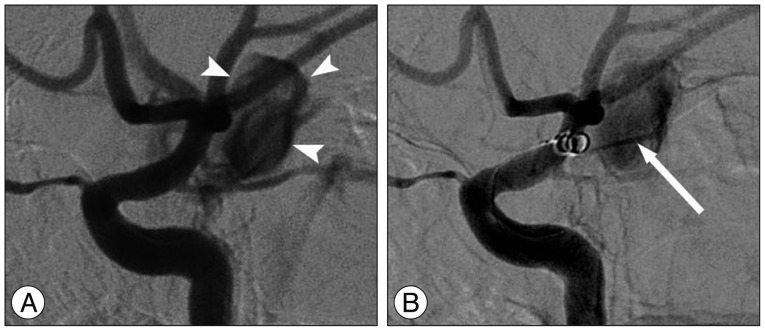
Fig.В 3
A simulation of the patient's situation in the brain using a fresh-frozen male cadaver (A) and computer graphics (B). The right anterior cerebral arteries (*) were removed to expose the AChAs and the frontal lobes are retracted posteriorly with the head fully extended. The optico-carotid cisterns are widened by the effect of gravity and retraction of the frontal lobes with the stretch of the AChA. When the optic tract is dragged backward with a retractor, the AChA is more stretched to be thinner and tensor. A schematic drawing shows typically the anatomic change in the AChA according to those situations (B). AChA : anterior choroidal artery. 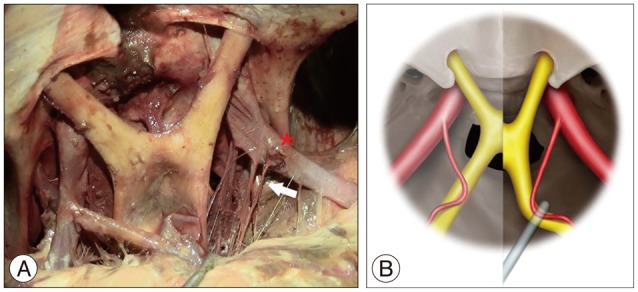
|
|