Lee, Chun, Yi, Bak, Ko, and Lee: Perioperative Risk Factors Related to Lumbar Spine Fusion Surgery in Korean Geriatric Patients
Abstract
Objective
Life expectancy for humans has increased dramatically and with this there has been a considerable increase in the number of patients suffering from lumbar spine disease. Symptomatic lumbar spinal disease should be treated, even in the elderly, and surgical procedures such as fusion surgery are needed for moderate to severe lumbar spinal disease. However, various perioperative complications are associated with fusion surgery. The aim of this study was to examine perioperative complications and assess risk factors associated with lumbar spinal fusion, focusing on geriatric patients at least 70 years of age in the Republic of Korea.
Methods
We retrospectively investigated 489 patients with various lumbar spinal diseases who underwent lumbar spinal fusion surgery between 2003 and 2007 at our institution. Three fusion procedures and the number of fused segments were analyzed in this study. Chronic diseases were also evaluated. Risk factors for complications and their association with age were analyzed.
Results
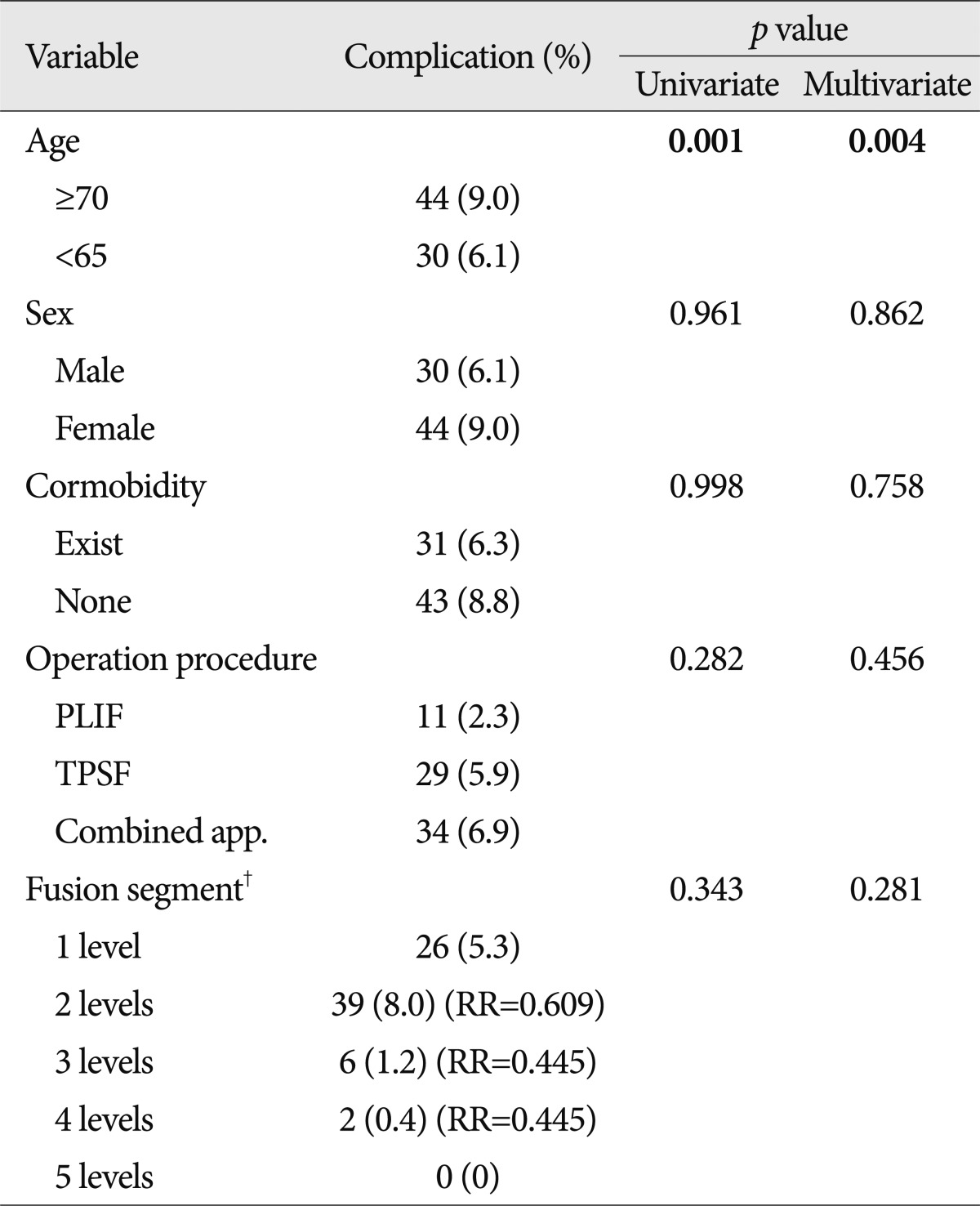
In this study, 74 patients experienced complications (15%). The rate of perioperative complications was significantly higher in patients 70 years of age or older than in other age groups (univariate analysis, p=0.001; multivariate analysis, p=0.004). However, perioperative complications were not significantly associated with the other factors tested (sex, comorbidities, operation procedures, fusion segments involved).
Conclusion
Increasing age was an important risk factor for perioperative complications in patients undergoing lumbar spinal fusion surgery whereas other factors were not significant. We recommend good clinical judgment and careful selection of geriatric patients undergoing lumbar spinal fusion surgery.
Key Words: Complication · Elderly patients · Lumbar spinal fusion.
INTRODUCTION
Life expectancy has dramatically increased as a result of several factors including improved nutritional support, advanced quality of life, and development of medical and surgical techniques. As the population of the world is aging, the number of patients suffering from lumbar spine disease has increased considerably, especially within the Republic of Korea. In addition, newly developed imaging equipment facilitates more sensitive and wider diagnosis of various disease entities.
The pathophysiologic and anatomic changes associated with the degenerative process include thickening of the ligaments, enlargement or loosening of the facet joints, and loss of water from discs 28). These changes may lead to a narrowing of the spinal canal and segmental instability with subsequent compression of the neural elements 28). In addition, elderly people are more vulnerable to external forces as a result of senile or postmenopausal osteoporosis, decreased pliability, and weakness of muscle tone. For these reasons, lumbar spinal diseases are commonly observed in the elderly. Although spinal disorders are not typically regarded as life threatening, they can lead to chronic pain and significant limitation of activity 15). Therefore, symptomatic lumbar spinal disease should be treated irrespective of patient age. An accurate assessment of the potential morbidities associated with spinal procedures is necessary to guide treatment 41). Conservative treatment such as medication, physical therapy, and steroid injection may relieve the symptoms in some cases 48). However, surgical treatment, and even fusion surgery, is typically needed for medically refractory cases with moderate to severe lumbar spinal disease. The majority of the elderly population has the concomitant problem of associated comorbidities. Advanced patient age, medical comorbidities, nutritional needs, life expectancy, and bone quality are important issues to consider when discussing spine surgery in the elderly. Many previous studies have emphasized the morbidity associated with surgical treatment of lumbar spinal disease in the elderly 10,24) and have recommended non-surgical treatment for elderly patients 22). Consequently, spine surgery in the elderly has generally been thought to be associated with an increased risk of perioperative complications. However, several authors recently claimed that surgical treatment of the elderly is both safe and efficacious because of newly developed surgical techniques and improved instruments 36,45). Ragab et al. 36) studied the safety and outcome of lumbar spinal surgery in patients 70 years of age or older and found that surgical treatment of lumbar spinal diseases in the elderly has a high success rate and satisfaction level, with results comparable to those in a younger population. Many previous reports focused on outcome assessments of specific procedures or diagnoses or outcomes as a function of age distribution 19,37,39,40). This study systematically analyzed previously reported risk factors in Korean patients. The aim of the study was to examine perioperative complications and assess the risk factors associated with lumbar spinal fusion, focusing on geriatric patients at least 70 years of age.
MATERIALS AND METHODS
Patient population
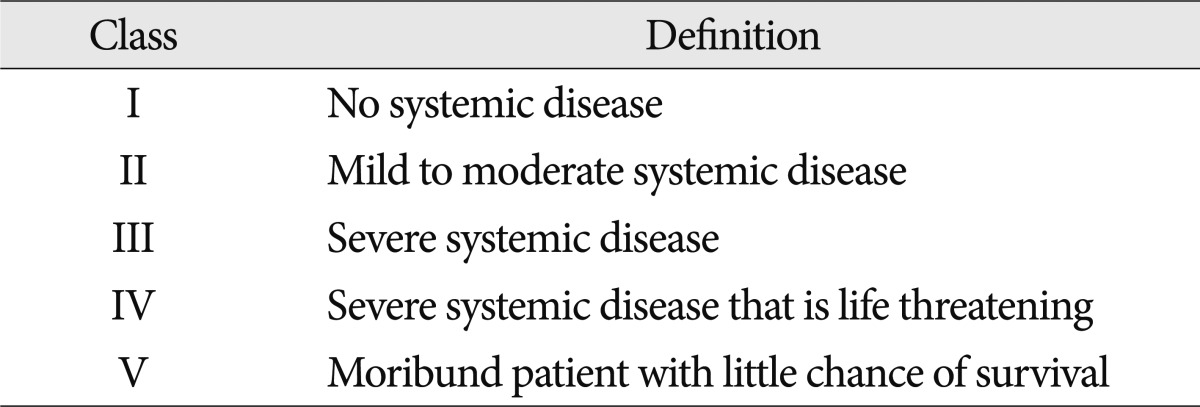
The present study included 489 patients who underwent lumbar spine fusion surgery (LSFS) from 2003 to 2007. Exclusion criteria were age between 66 and 69 years, decompression only, anterior interbody fusion, a follow-up period less than 12 months, and severe co-morbidity [American Society of Anesthesiologists (ASA) classification of physical status >III] ( Table 1). LSFS was performed by one neurosurgeon at a single institute, Hanyang University Medical Center. The patients were divided according to the definition of 'geriatric' into group 1 (older than 70 years) and group 2 (younger than 65 years). We enrolled patients with various preoperative diagnoses including degenerative spine disease, spine trauma, and revision surgery after the previously mentioned diseases, and excluded patients suffering from spine tumors to avoid unexpected co-morbidities. Data related to these patients were evaluated by a single observer using the standard hospital chart, outpatient notes, electronic medical records, operative reports, and preoperative and postoperative imaging studies. The following demographic variables were evaluated : principal diagnosis, previous spine surgery, treatable or non-treatable medical co-morbidities, bone mineral density (BMD), surgical approach, and segment of fusion.
Radiological evaluation
Preoperative plain radiographs including anteroposterior (AP), lateral, both oblique, and dynamic views (flexion and extension) were obtained for all patients except those with traumatic lesions, who were evaluated with only AP and lateral views. Additionally, all enrolled patients underwent magnetic resonance imaging and computed tomography (CT) scanning of the lumbar lesion preoperatively. Plain radiographs with AP and lateral views were obtained immediately after surgery, and then at 1, 3, 6, and 12 months thereafter. Additional CT scans were performed as follow-up to evaluate perioperative complications as needed.
Co-morbidities
All patients were evaluated for co-morbidities such as cardiovascular, renal, pulmonary, and endocrine problems. Co-morbidities were subdivided as follows : cardiovascular (hypertension, coronary artery disease, and congestive heart failure), renal disease (renal cyst and acute or chronic renal failure), pulmonary (chronic obstructive pulmonary disease and asthma), endocrine (hyperthyroidism, hypothyroidism, and diabetes mellitus), liver disease (fatty liver, liver cyst, hepatitis, liver cirrhosis), rheumatoid arthritis, peptic ulcer disease, and others.
Surgical treatment
We performed several types of fusion surgery according to the patient's lumbar spine disease. In general, surgery was performed in degenerative cases when conservative treatment over three months failed to improve the patient's symptoms. We used three different surgical approaches: trans-pedicular screw fixation (TPSF), posterior lumbar interbody fusion (PLIF), and a combined approach. In the present study, all techniques were used interchangeably by the two neurosurgeons. In patients who only underwent TPSF, postero-lateral fusion was simultaneously performed at the intertransverse process space with autologous lamina bone and an allograft.
Postoperative care
Patients were ambulated from postoperative day 2 with a rigid molded plastic brace or lumbar corset. Patients were initially treated with analgesia for control of acute pain by intravenous injection, and then quickly weaned to mild oral narcotic therapy and NSAIDs that were discontinued as soon as possible.
Complications
The term "complication" is broadly and differently defined in the published literature. In this study, a complication was defined as any event requiring specific management during the perioperative period, including the intra-operative and post-operative periods. Based on a PubMed search of previous literature with the keyword "complication," we considered the following to be complications : intra-operative complications such as dura tear, and postoperative complications including infection, spondylitis, hematoma accumulation, wound dehiscence or infection, mal-position of instrumentation, and aggravated neurologic symptoms when compared with preoperative status. However, postoperative systemic complications such as pneumonia, bowel ileus, or renal failure were excluded because they could be caused by any surgery with general anesthesia. All complications were verified by retrospective chart reviews. In addition, any need for reoperation during the follow-up period was noted, and the reason was recorded.
Evaluation of outcome
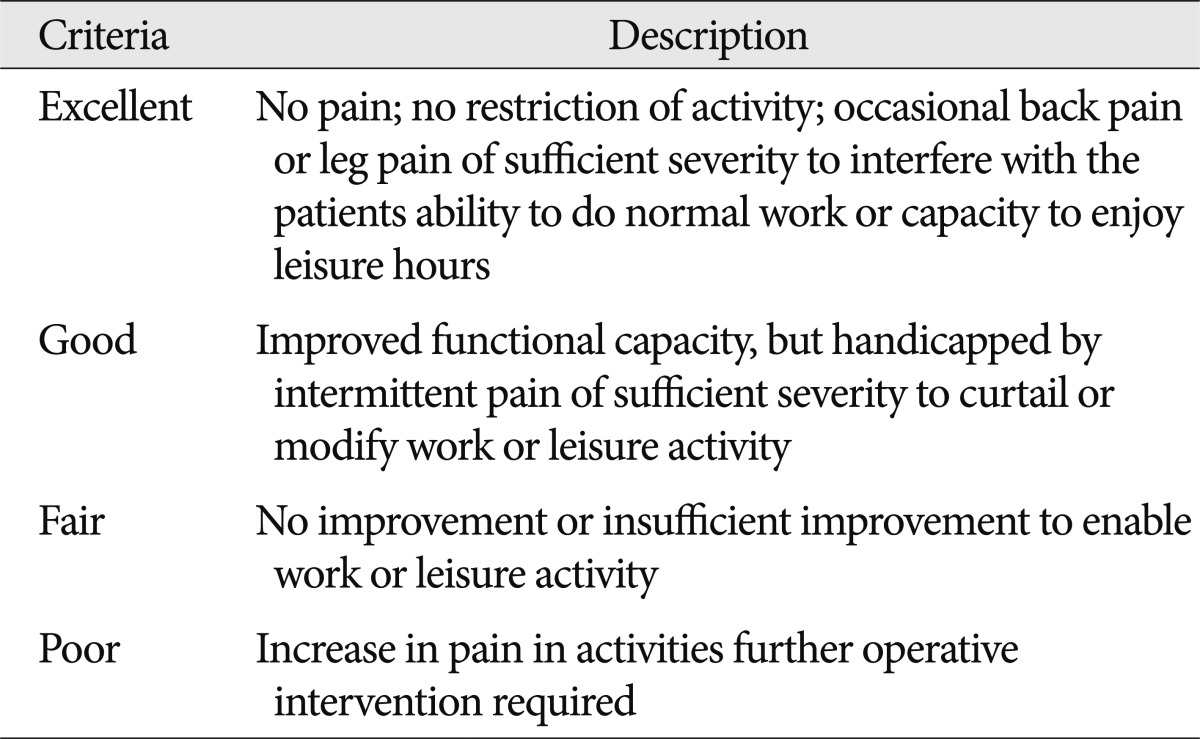
The patients enrolled in the present study were followed up for at least 12 months postoperatively. To evaluate objective neurologic improvement, we used the visual analogue scale (VAS) and MacNab's criteria ( Table 2).
Statistical analysis
Several univariate statistical analyses were performed to estimate the association among various factors as follows : Student's t-test for the analysis of relationships among BMD, age, and sex; chi-square test for age and underlying disease; and logistic regression models to determine the relationship between age and other factors with the occurrence of complications. Finally, we used binomial univariate logistic regression analysis to evaluate the correlation between the occurrence of complications and age, sex, preoperative diagnosis, comorbidities, ASA class, and procedural details. p-values <0.05 were considered statistically significant.
Variables significant on univariate analysis were further tested in multivariate logistic regression models. Multivariate generalized linear models were applied to assess the statistical significance of each individual variable while adjusting for other covariates. p-values <0.05 were considered significant. Because the focus of the present study was elderly patients, age was kept in the regression model throughout regardless of its significance. For each variable, ORs and 95% CIs were calculated. A predetermined subset analysis was performed to characterize complication rates according to age and to identify specific risk factors. Descriptive and procedural information were compiled, and complication rates were calculated according to the previously described definition. Univariate and multivariate logistic regression analyses were used to identify factors associated with complications in elderly patients. All statistical analyses were performed with SPSS statistical software version 16.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Patient population
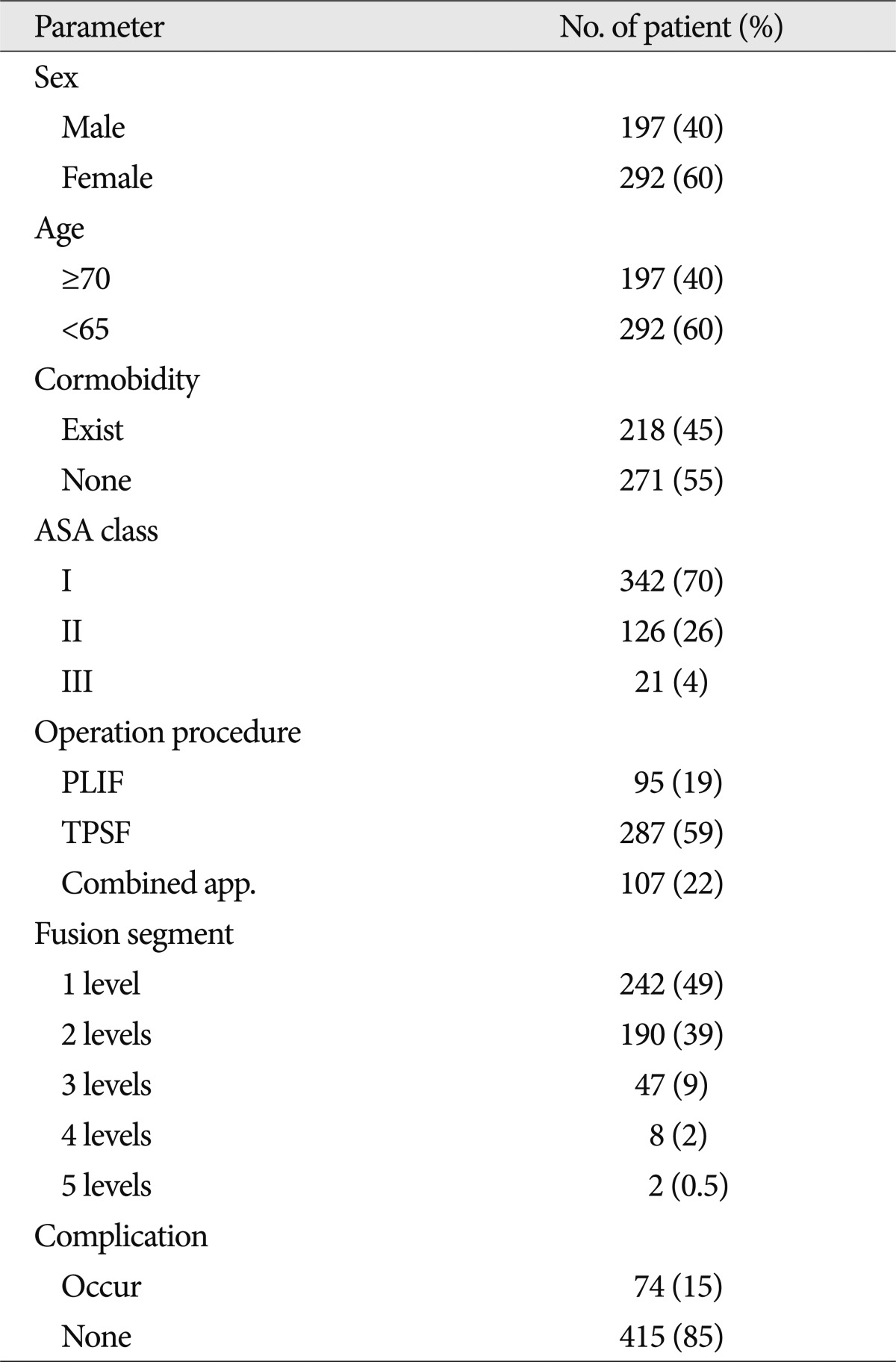
During the five-year study period, 489 patients who met the inclusion criteria underwent instrumented fusion surgery ( Table 3). Of these, 197 patients (40%) were male and 292 (60%) were female, and there were 197 patients (40%) in group 1 and 292 patients (60%) in group 2. The mean age was 57.8 years (group 1, 58.27 years; group 2, 75.91 years). The general condition of most patients was ASA class I (342 patients) or II (126 patients) with a few patients in ASA class III. The distribution of surgical procedures was as follows : 287 patients (59%) with TPSF, 95 patients (19%) with PLIF, and 107 patients (22%) with combined procedure. Single-level fusion surgery was performed in 242 patients (49%) whereas the remainder underwent a multi-segment procedure. The average fusion segment length was 1.64 segments. The most commonly treated levels were L4-5 and L3-4. Additionally, 45% of patients had comorbidities, and complications were encountered in 74 patients (15%).
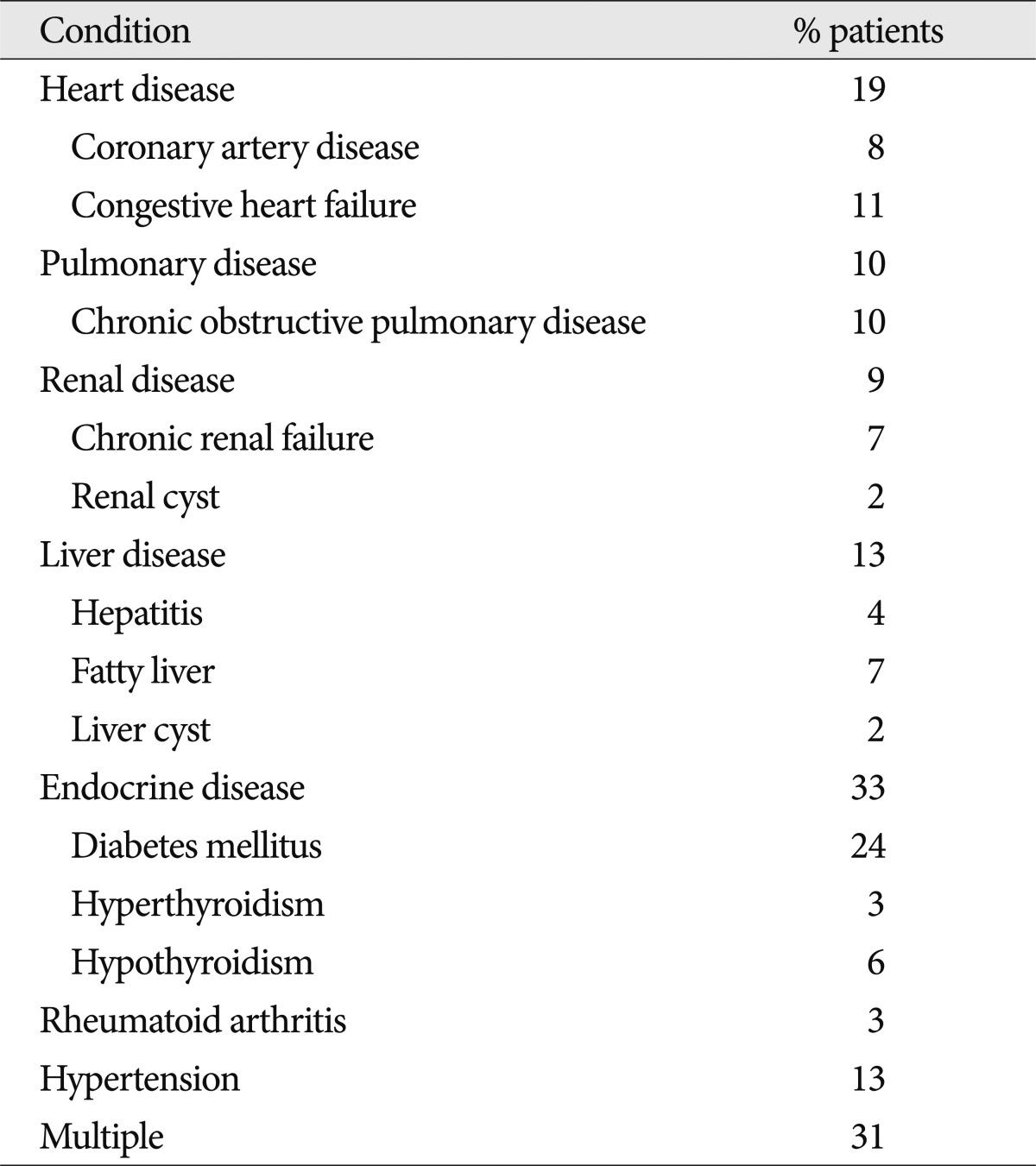
Comorbidities
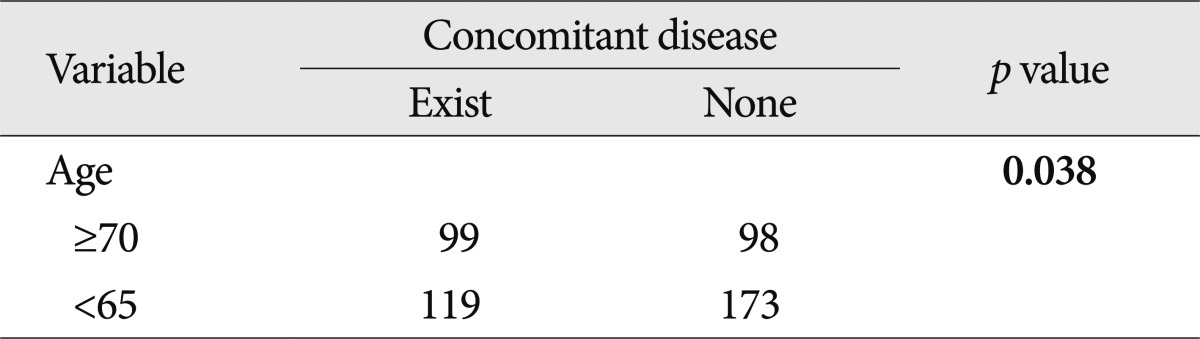
Among the observed comorbidities the most common problem was endocrine disease, which was present preoperatively in 33% of the patients. Endocrine disease was subdivided into diabetesmellitus (24%), hypothyroidism (6%), and hyperthyroidism (3%). Other comorbidities were cardiovascular disease (19%), hypertension (13%), liver disease (13%), pulmonary disease (10%), and renal disease (9%). In addition, 31% of the patients had more than one comorbidity ( Table 4). We also estimated the correlation between age and underlying disease. Almost half of the geriatric patients had underlying diseases and there was a statistically significant association between age and underlying disease ( p=0.038) ( Table 5).
Complications
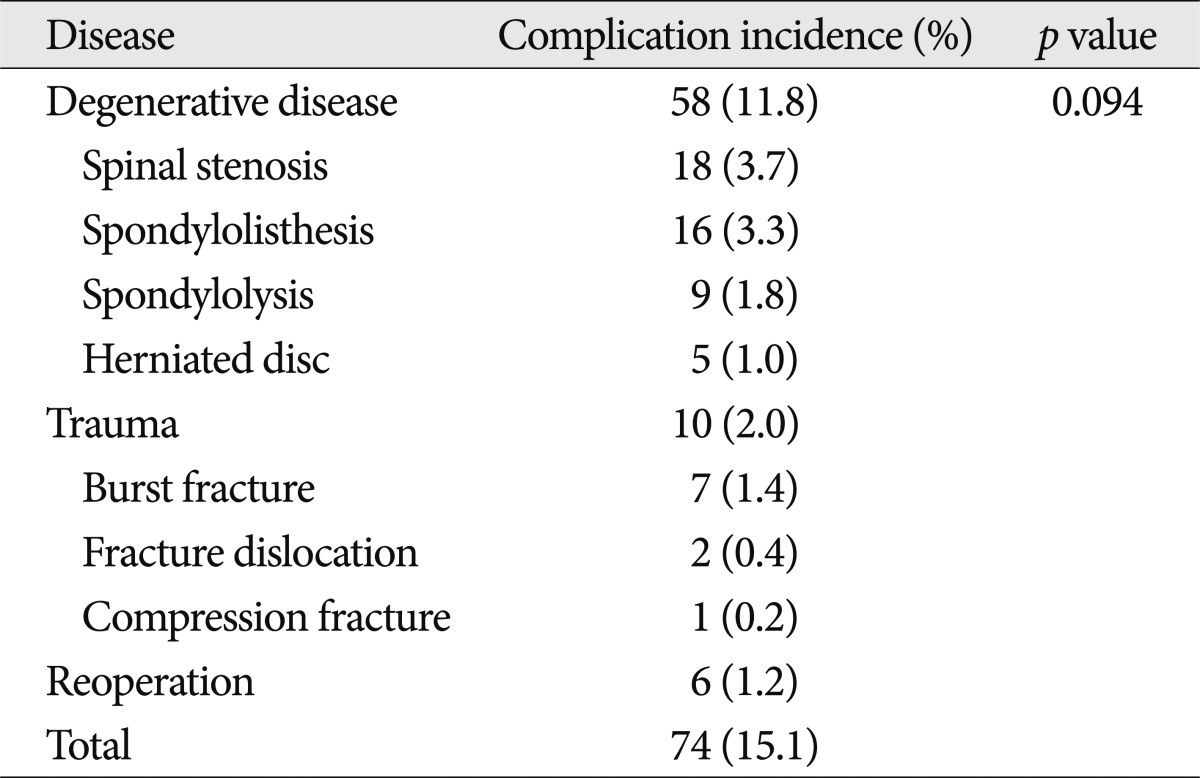
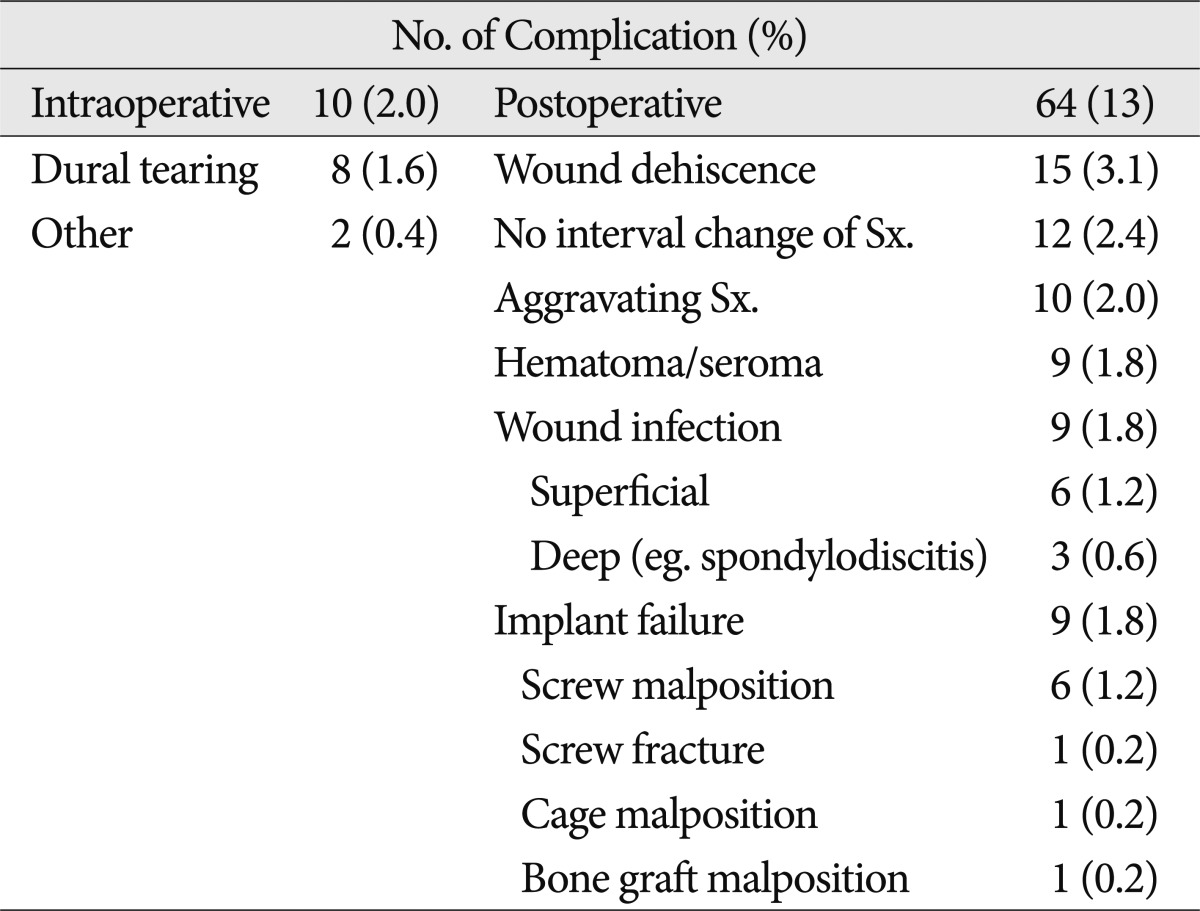
Although there was a trend toward increased incidence of complications in patients who underwent surgery for degenerative disease, there was no statistically significant correlation between diagnosis and overall complications. The overall incidence of degenerative disease, trauma, and reoperation was 11.8%, 2.0%, and 1.2%, respectively ( Table 6). Complications arising in the 74 patients are listed in Table 7. Intraoperative dura tearing occurred in 2.0% of the patients. The total postoperative complication rate in all patients was 13%, and the overall peri-operative complication rate in patients 70 years of age or older was 9%. Among these complications, 35 cases were re-treated (6 cases of dura tearing, 12 cases of wound dehiscence, 4 cases of hematoma accumulation, 6 cases of wound infection, and 7 cases of implant failure). The results of the logistic regression analysis are displayed in Table 8. Age was the only statistically significantly factor in both univariate and multivariate analyses ( p=0.001 and 0.004). Other factors such as sex, comorbidities, and operation procedure were not statistically significant. In addition, a greater number of fusion segments was not predictive of complications.
Osteoporosis
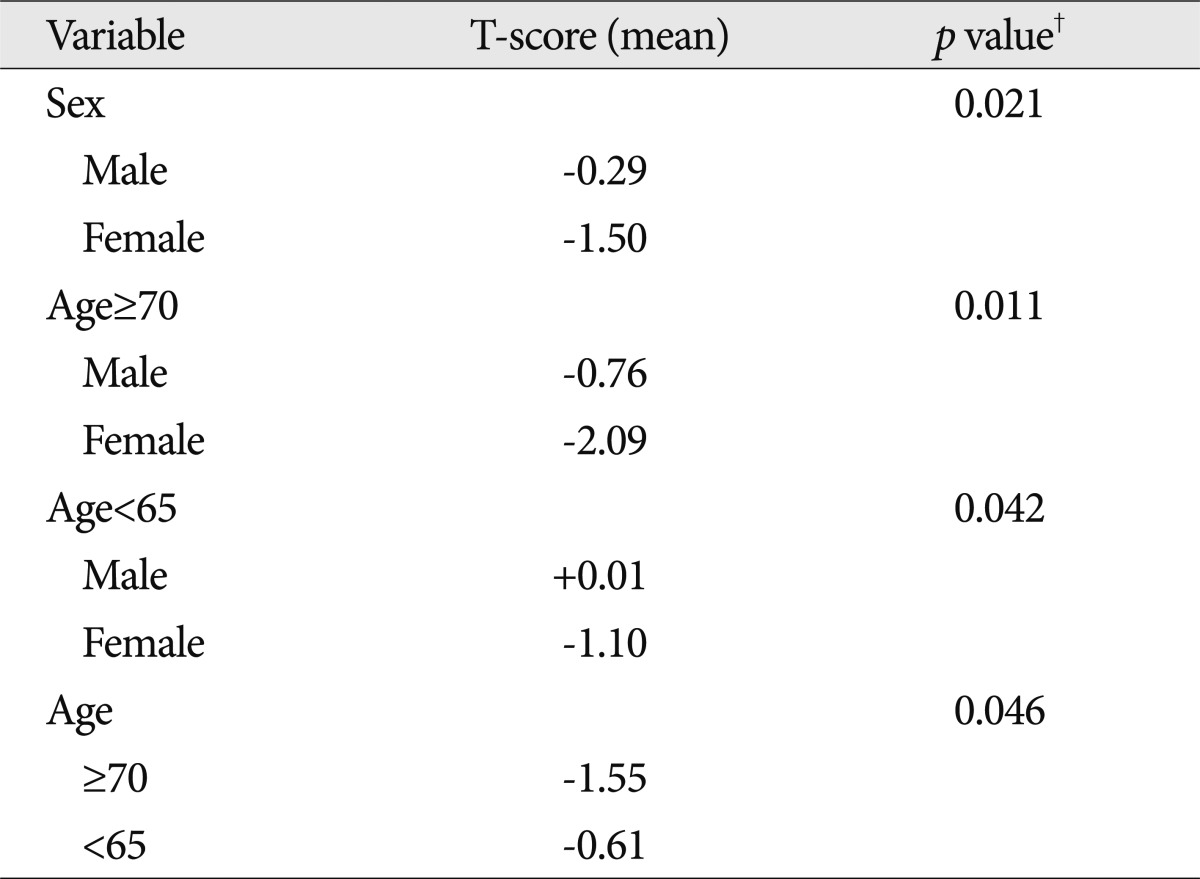
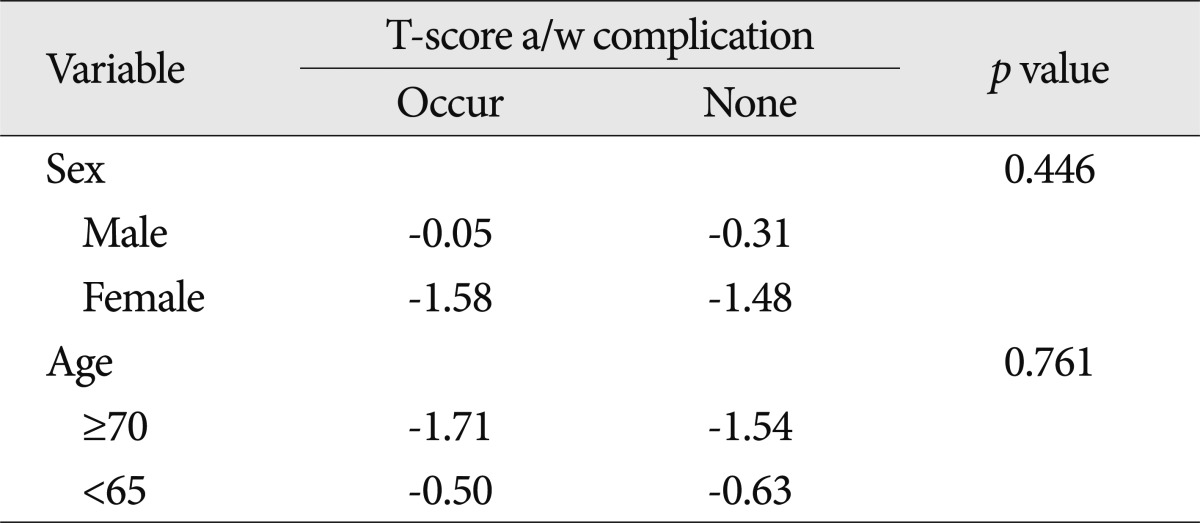
According to the present data, older patients and female patients had a lower T-score than younger patients and male patients on univariate analysis ( Table 9). However, there was no statistically significant relationship between low bone mineral density and perioperative complications ( p=0.446 for sex and 0.761 for age) ( Table 10).
Neurologic symptoms
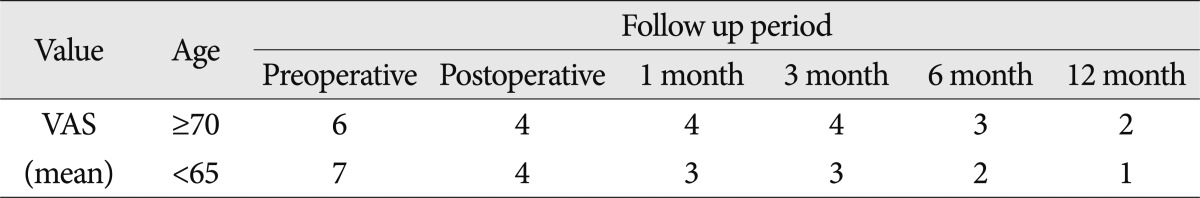
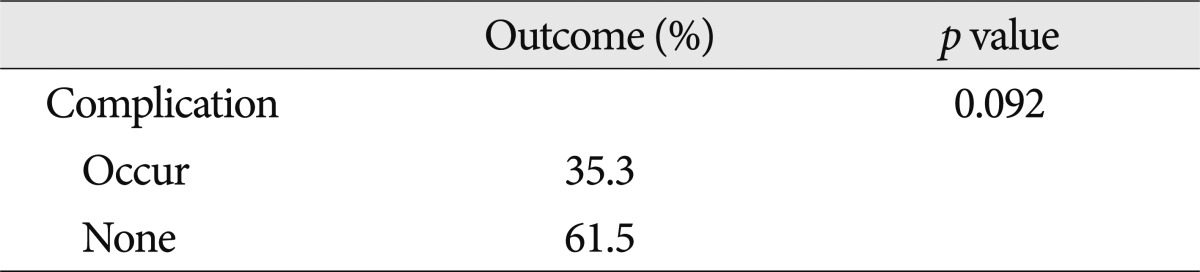
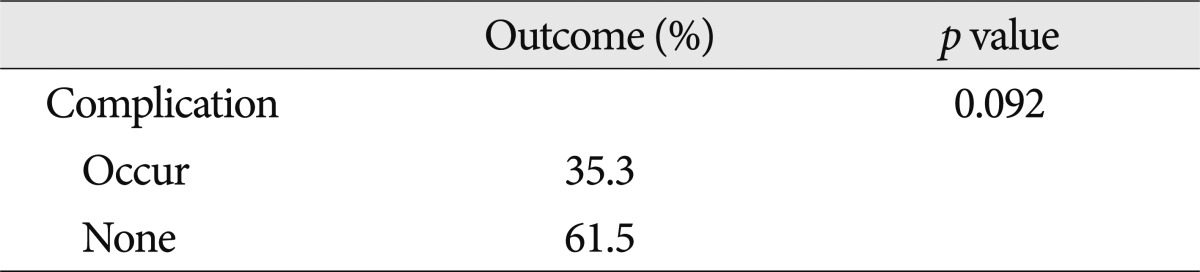
Preoperatively, the mean VAS was six points in geriatric patients and seven points in younger patients. However, the final VAS was two in older patients and one in younger patients. There was a statistically significant difference between the two groups. Based on the mean MacNab criteria, both groups had good outcomes ( Table 11). Worsening or maintenance of the preoperative status during the course of the follow-up period was seen in 17 (3.4%) of the 489 patients and was generally attributed to back pain, radiating pain to the leg, or neurogenic claudication. The remaining patients had relief of approximately 57.5% of their symptoms compared with preoperative status. There was no significant correlation with age, comorbidities, operation procedure, and fusion segment. In addition, there was no statistically significant relationship between perioperative complications and neurologic outcome ( p=0.092) ( Table 12).
DISCUSSION
The number of elderly persons in the Republic of Korea continues to grow, with an expected 38.2% of people older than 65 years by the year 2050. This greatly exceeds the worldwide mean of 16.2%. An aging population will suffer from age-related degenerative diseases, such as disorders of the spine. Today, elderly people live longer, have more active lifestyles, and have a great desire to be pain free throughout the last decades of life. Advances in anesthesiology, spinal instrumentation, and post-operative care have made spinal procedures safer, with a decrease in morbidity and mortality and improved patient outcomes 7). Additionally, they have allowed more extensive and complex procedures to be performed in at-risk populations, such as the elderly 7). Identifying predictors of complications or poor outcome in the geriatric population is important for perioperative risk assessment and for implementing appropriate preventative measures. There is no standard definition of "complication" in the spine literature 37). Various classification systems have been used, often to suit the investigator, making analysis and comparison of the literature difficult 8,37,39,43). In the current study, a previously validated classification of complications was not used. Most previous studies in the literature used a binary system, and included systemic complications associated with surgery 38). In the present study, however, we did not choose a binary system of complications and excluded systemic complications because it was unclear whether systemic complications occurring in the perioperative period were related to spine surgery. The incidence of complications in this current analysis was 15.1%, which is a little lower than that in several previous retrospective studies 2,10,33,46). In a review of 105 spine surgery articles, Nasser et al. 30) reported an overall pooled complication incidence of 16.4%. The most common perioperative complication observed in this study was wound dehiscence, at a rate of 2.6%, while laceration of the dura was the most common intraoperative complication (1.6%). Reoperation after spinal fusion surgery may be considered a failure of the initial surgery by the patient and surgeon and represents an additional procedure in patients who are already at significant risk for complication 7). Mok et al. 27) recently evaluated the need for revision surgery in patients undergoing adult spine surgery, finding a cumulative rate of 25.8%, while Cloyd et al. 7) reported a reoperation rate of 27.4% in patients at least 65 years old who presented with a wide range of spine pathologies. In this study, the rate of revision surgery due to complications was approximately 47%, but age was not associated with the need for reoperation. Cloyd et al. 7) found that age is a risk factor for major postoperative complications with an OR of 1.04 ( p=0.039). A ten-year increase in age is associated with a 48% greater risk for a major postoperative complication. An alarming 24.2% of elderly patients incur a major postoperative complication and 53.2% experienced at least one in-hospital complication. The rates of complications for spinal arthrodesis in elderly patients are highly variable, ranging from 14 to 80% 4,5,26,31,35). Okuda et al. 31) found that patients older than 70 years who had undergone posterior lumbar interbody fusion for spondylolisthesis had a complication rate of 16%, which was not significantly different from that in younger patients; however, these authors admittedly excluded minor complications from their analysis. Kilinçer et al. 26) also found that age did not affect the complication rates of posterior lumbar interbody fusion, but they did not report a complication rate separately for older patients. Vitaz et al. 45) found that elderly patients with lumbar spinal disease can be surgically treated in a similar fashion to younger patients. On the other hand, Deyo et al. 10) retrospectively analyzed a statewide hospital discharge registry and compiled data on more than 18000 hospitalizations over a two-year period. Patients with nondegenerative pathologies were excluded from the analysis. These authors reported an overall complication rate of only 10.3% for the surgical treatment of degenerative lumbar spine disease, although the rate for patients older than 75 years was higher (18%). Our data also showed a difference between the older and younger groups; the complication rate of the older group was 9%, while that of the younger group was 6%. There was a statistically significant association between age and perioperative complications (univariate analysis, p=0.001; multivariate analysis, p=0.004). The relationship between comorbidities and surgical outcome has historically been controversial. Early studies investigating the effect of age on decompression with fusion for lumbar stenosis found that the presence of multiple comorbidities was associated with perioperative complications 24,32,43). Katz et al. 24) found that greater cardiovascular, musculoskeletal, and overall comorbidities led to poorer scores in most of the outcome measurements. However, for lumbar spinal fusion in the elderly, several recent studies have found the opposite to be true 1,2,4,5,26). Although Daubs et al. 9) did not find an association between comorbidities and complications, it is unclear whether they only studied the effect of individual diseases or the total number of comorbidities. The results of our study indicate that for lumbar fusions in the elderly, the number of comorbidities is not associated with perioperative complications (univariate analysis, p=0.998; multivariate analysis, p=0.758). Sanjay et al. 47) found no correlation between diagnosis and overall incidence of complications ( p=0.08), although a trend toward increased complications in patients undergoing surgery for neoplastic or infectious pathology was observed. In this subset of the patient population, patients with preoperative diagnoses of infection and neoplasm were more often affected by isolated and multiple complications ( p=0.05 and p=0.02, respectively). Patil et al. 33) reviewed 26233 admissions for patients with surgically managed spine metastases from the National Inpatient Sample, a public database maintained by the Agency for Healthcare Research and Quality and found a higher complication rate in elderly patients. In this series, however, there was no statistically significant association between primary diagnosis and the rate of complication ( p=0.094). Previous studies have suggested a higher incidence of complications with revision surgery compared with primary surgery 2,18,43), possibly because scar tissue from the previous surgery may deform anatomy and increase the risk of injury to vascular structures, soft tissues, or visceral organs 8). It may also affect wound healing and increase the risk of surgical site infections. Sidhu et al. 43) found that the complication rate of revision lumbar surgery was three to five times higher than the reported rates for primary surgery. In that study, the overall complication rate for revision surgery at the same operative level was 42%. However, in the current study, the complication rate of 1.2% for reoperation was lower than that for primary surgery (14%). Several studies have shown increased rates of complication with fusion versus non-fusion procedures 6,16,23). Fusion and instrumentation surgeries are generally more complex than non-fusion surgeries and the potential for injury and infection may be greater 41). However, the indications for lumbar fusion in the treatment of spine segment instability due to various causes remain controversial 11). Our indications for lumbar spinal fusions have included severe low back pain 25,49), mechanical or iatrogenic spinal instability 3,14,18), degenerative spondylolisthesis 12,13,29,34,44), and traumatic lumbar spinal injury. In our practice the decision to perform spinal fusion with instrumentation is based on the individual patient. Part of this consideration includes the patient's overall health status and ability to withstand a longer operation. Some authors believe that pedicle screw or rod fixation-type fusion procedures have become the gold standard for arthrodesis 11). These procedures obviate the extensile exposure required for intertransverse fusion procedures and require less bone graft material, thereby minimizing donor-site morbidity and complications. It has also been proposed that interbody fusion offers restoration of load-bearing capacity to the ventral spinal column and maintenance of interspace disc height, and that the smaller exposure results in fewer complications 11). In this study, a significant association was not detected between fusion type and risk of perioperative complications in patients of all ages, including the elderly (univariate analysis, p=0.282; multivariate analysis, p=0.456). Elderly patients who present with symptomatic spinal pathology may require single or extensive lumbar fusions to ensure adequate fusion and prevent future instrumentation-related complications 7). Several studies have suggested that longer fusion lengths lead to an increased risk of complications in the elderly 4,5,35). Carreon et al. 4) found an OR of 2.4 for postoperative complications in older patients undergoing lumbar arthrodesis with instrumentation. Similarly, Casinelli et al. 5) found that fusion of four or more segments was predictive of complications. The mean number of levels fused in these studies was 2.4 and 1.9, respectively. On the other hand, Daubs et al. 9) studied patients older than 60 years who underwent spinal arthrodesis with a mean of 9.1 levels fused and found no association between the length of fusion and complication risk. Moreover, Glassman et al. 17) found that extending the fusion length may actually offer improved clinical outcomes in the setting of poor sagittal balance or spinal cord compression. Elderly patients may require extensive multilevel thoracolumbar spinal fusion procedures for a variety of indications, such as to restore sagittal balance, revise failed constructs, debride infections, or resect large spinal tumors 7). In our study, there was no significant association between the number of segments fused and the risk of perioperative complications in patients of all ages, including the elderly (univariate analysis, p=0.343; multivariate analysis, p=0.281). We therefore believe that the number of fusion segments may be not significantly associated with perioperative complications in lumbar spinal fusion surgery, therefore fusion extension should be determined by the surgeon as the occasion demands. While the findings of the current study are important, there are several limitations. First, this study is a retrospective analysis, for which the limitations are well known. Retrospective studies may underestimate the actual complication incidence through the introduction of investigator recall bias 21,42). A disproportionate reliance on the memory of different investigators and the accuracy of medical records may lead to falsely low reported rates of complication 21). Differences in the interpretation of the patients' degree of pain and neurologic examinations may also lead to a biased result. Second, there are several other opportunities for bias in the present study. There was significant case complexity in our patient population; thus the current study population may not represent the spine surgery population as a whole. Therefore, these findings may not be generalizable to a wider group of spinal fusion surgery patients. Third, we used our own definition of spinal fusion surgery complications. This definition may not represent the views of all spine surgeons, and inclusion of adverse medical events may not be an acceptable methodology to the general spine surgery community.
CONCLUSION
The number of spinal fusion surgeries performed for lumbar spinal disease has increased due to improved surgical techniques and advances in medical treatment, including anesthesia. However, various complications are associated with fusion surgery. The incidence of complications in this series is similar to that in previously published papers. In this study, increasing age was an important risk factor for perioperative complications in patients undergoing lumbar spinal fusion surgery. There was no significant difference between the various procedures in terms of outcome. The general condition of patients with respect to a number of chronic diseases did not affect the risk of perioperative complications. An important finding of the present study is that the occurrence of complications did not affect clinical outcome. Therefore, if good clinical judgment and careful patient selection are applied, fusion surgery may be performed in geriatric patients, even in those with many concomitant diseases.
Acknowledgements
This work was supported by the research funding of Hanyang University (HY-2011-N). Institutional Review Board was approved by Hanyang University Medical Center (HYUH-IRB-2011-R-35). This manuscript has been reviewed and corrected by English editorial services and statistical service of Hanyang University Medical Service Center.
References
1. Benz RJ, Ibrahim ZG, Afshar P, Garfin SR : Predicting complications in elderly patients undergoing lumbar decompression. Clin Orthop Relat Res 2001, 116-121,  2. Boakye M, Patil CG, Ho C, Lad SP : Cervical corpectomy : complications and outcomes. Neurosurgery 2008, 63 : 295-301; discussion 301-302,   3. Caputy AJ, Luessenhop AJ : Long-term evaluation of decompressive surgery for degenerative lumbar stenosis. J Neurosurg 1992, 77 : 669-676,   4. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR : Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 2003, 85 : 2089-2092,   5. Cassinelli EH, Eubanks J, Vogt M, Furey C, Yoo J, Bohlman HH : Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis : an analysis of 166 patients. Spine (Phila Pa 1976) 2007, 32 : 230-235,   6. Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, et al : Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007, 32 : 2232-2237,   7. Cloyd JM, Acosta FL Jr, Cloyd C, Ames CP : Effects of age on perioperative complications of extensive multilevel thoracolumbar spinal fusion surgery. J Neurosurg Spine 2010, 12 : 402-408,   8. Daniels AH, Riew KD, Yoo JU, Ching A, Birchard KR, Kranenburg AJ, et al : Adverse events associated with anterior cervical spine surgery. J Am Acad Orthop Surg 2008, 16 : 729-738,   9. Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH : Adult spinal deformity surgery : complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007, 32 : 2238-2244,   10. Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA : Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am 1992, 74 : 536-543,   11. Elias WJ, Simmons NE, Kaptain GJ, Chadduck JB, Whitehill R : Complications of posterior lumbar interbody fusion when using a titanium threaded cage device. J Neurosurg 2000, 93 : 45-52,   12. Esses SI, Huler RJ : Indications for lumbar spine fusion in the adult. Clin Orthop Relat Res 1992, 87-100,   13. Feffer HL, Wiesel SW, Cuckler JM, Rothman RH : Degenerative spondylolisthesis. To fuse or not to fuse. Spine (Phila Pa 1976) 1985, 10 : 287-289,   14. Frazier DD, Lipson SJ, Fossel AH, Katz JN : Associations between spinal deformity and outcomes after decompression for spinal stenosis. Spine (Phila Pa 1976) 1997, 22 : 2025-2029,   15. Garfin SR, Mirkovic S, Herkowitz HN : Spinal stenosis: indications for laminectomy. Instr Course Lect 1994, 43 : 411-414,  16. Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR : Perioperative complications of lumbar instrumentation and fusion in patients with diabetes mellitus. Spine J 2003, 3 : 496-501,   17. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR : Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005, 30 : 682-688,   18. Gumbs AA, Hanan S, Yue JJ, Shah RV, Sumpio B : Revision open anterior approaches for spine procedures. Spine J 2007, 7 : 280-285,   19. Haid RW Jr, Subach BR, McLaughlin MR, Rodts GE Jr, Wahlig JB Jr : C1-C2 transarticular screw fixation for atlantoaxial instability : a 6-year experience. Neurosurgery 2001, 49 : 65-68; discussion 69-70,   20. Hanley EN Jr : The indications for lumbar spinal fusion with and without instrumentation. Spine (Phila Pa 1976) 1995, 20 : 143S-153S,   21. Hess DR : Retrospective studies and chart reviews. Respir Care 2004, 49 : 1171-1174,  22. Johnsson KE, Rosén I, Udén A : The natural course of lumbar spinal stenosis. Clin Orthop Relat Res 1992, 82-86,   23. Katz JN : Lumbar spinal fusion. Surgical rates, costs, and complications. Spine (Phila Pa 1976) 1995, 20 : 78S-83S,   24. Katz JN, Lipson SJ, Larson MG, McInnes JM, Fossel AH, Liang MH : The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg Am 1991, 73 : 809-816,   25. Katz JN, Lipson SJ, Lew RA, Grobler LJ, Weinstein JN, Brick GW, et al : Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis. Patient selection, costs, and surgical outcomes. Spine (Phila Pa 1976) 1997, 22 : 1123-1131,   26. Kilinçer C, Steinmetz MP, Sohn MJ, Benzel EC, Bingaman W : Effects of age on the perioperative characteristics and short-term outcome of posterior lumbar fusion surgery. J Neurosurg Spine 2005, 3 : 34-39,   27. Mok JM, Cloyd JM, Bradford DS, Hu SS, Deviren V, Smith JA, et al : Reoperation after primary fusion for adult spinal deformity : rate, reason, and timing. Spine (Phila Pa 1976) 2009, 34 : 832-839,   28. Morgalla MH, Noak N, Merkle M, Tatagiba MS : Lumbar spinal stenosis in elderly patients : is a unilateral microsurgical approach sufficient for decompression? J Neurosurg Spine 2011, 14 : 305-312,   29. Mullin BB, Rea GL, Irsik R, Catton M, Miner ME : The effect of postlaminectomy spinal instability on the outcome of lumbar spinal stenosis patients. J Spinal Disord 1996, 9 : 107-116,   30. Nasser R, Yadla S, Maltenfort MG, Harrop JS, Anderson DG, Vaccaro AR, et al : Complications in spine surgery. J Neurosurg Spine 2010, 13 : 144-157,   31. Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M : Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am 2006, 88 : 2714-2720,   32. Oldridge NB, Yuan Z, Stoll JE, Rimm AR : Lumbar spine surgery and mortality among Medicare beneficiaries, 1986. Am J Public Health 1994, 84 : 1292-1298,    33. Patil CG, Lad SP, Santarelli J, Boakye M : National inpatient complications and outcomes after surgery for spinal metastasis from 1993-2002. Cancer 2007, 110 : 625-630,   34. Porter RW : Spinal stenosis and neurogenic claudication. Spine (Phila Pa 1976) 1996, 21 : 2046-2052,   35. Raffo CS, Lauerman WC : Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976) 2006, 31 : 99-103,   36. Ragab AA, Fye MA, Bohlman HH : Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine (Phila Pa 1976) 2003, 28 : 348-353,   37. Rampersaud YR, Moro ER, Neary MA, White K, Lewis SJ, Massicotte EM, et al : Intraoperative adverse events and related postoperative complications in spine surgery : implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976) 2006, 31 : 1503-1510,   38. Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, et al : Complications in spinal surgery : comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine 2009, 10 : 578-584,   39. Rihn JA, Patel R, Makda J, Hong J, Anderson DG, Vaccaro AR, et al : Complications associated with single-level transforaminal lumbar interbody fusion. Spine J 2009, 9 : 623-629,   40. Romano PS, Campa DR, Rainwater JA : Elective cervical discectomy in California: postoperative in-hospital complications and their risk factors. Spine (Phila Pa 1976) 1997, 22 : 2677-2692,   41. Sauerland S, Lefering R, Neugebauer EA : Retrospective clinical studies in surgery : potentials and pitfalls. J Hand Surg Br 2002, 27 : 117-121,   42. Schwender JD, Casnellie MT, Perra JH, Transfeldt EE, Pinto MR, Denis F, et al : Perioperative complications in revision anterior lumbar spine surgery : incidence and risk factors. Spine (Phila Pa 1976) 2009, 34 : 87-90,   43. Sidhu KS, Herkowitz HN : Spinal instrumentation in the management of degenerative disorders of the lumbar spine. Clin Orthop Relat Res 1997, 39-53,  44. Smith EB, Hanigan WC : Surgical results and complications in elderly patients with benign lesions of the spinal canal. J Am Geriatr Soc 1992, 40 : 867-870,   45. Vitaz TW, Raque GH, Shields CB, Glassman SD : Surgical treatment of lumbar spinal stenosis in patients older than 75 years of age. J Neurosurg 1999, 91 : 181-185,   46. Wang MC, Chan L, Maiman DJ, Kreuter W, Deyo RA : Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine (Phila Pa 1976) 2007, 32 : 342-347,   47. Yadla S, Malone J, Campbell PG, Maltenfort MG, Harrop JS, Sharan AD, et al : Early complications in spine surgery and relation to preoperative diagnosis : a single-center prospective study. J Neurosurg Spine 2010, 13 : 360-366,   48. Yamashita K, Ohzono K, Hiroshima K : Five-year outcomes of surgical treatment for degenerative lumbar spinal stenosis: a prospective observational study of symptom severity at standard intervals after surgery. Spine (Phila Pa 1976) 2006, 31 : 1484-1490,   49. Yone K, Sakou T, Kawauchi Y, Yamaguchi M, Yanase M : Indication of fusion for lumbar spinal stenosis in elderly patients and its significance. Spine (Phila Pa 1976) 1996, 21 : 242-248,  
Table 1
The American Society of Anesthesiologists classification of physical status 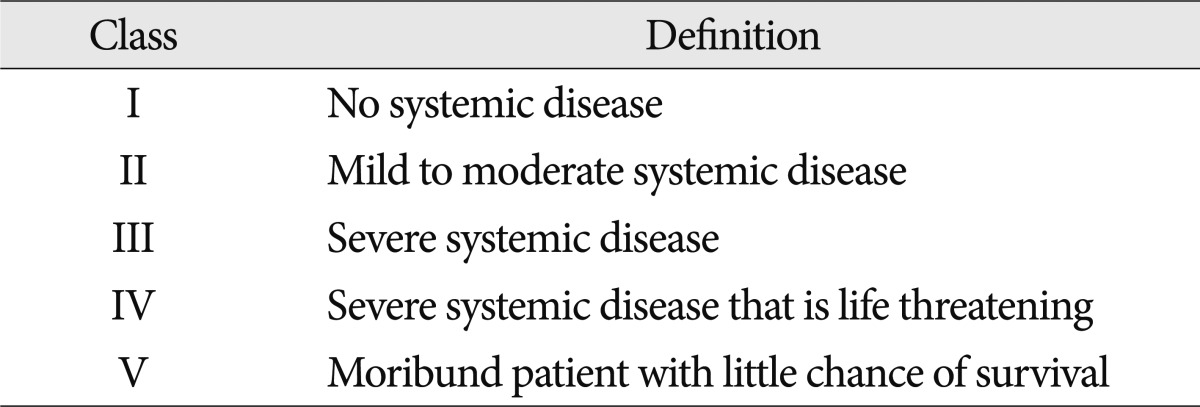
Table 2
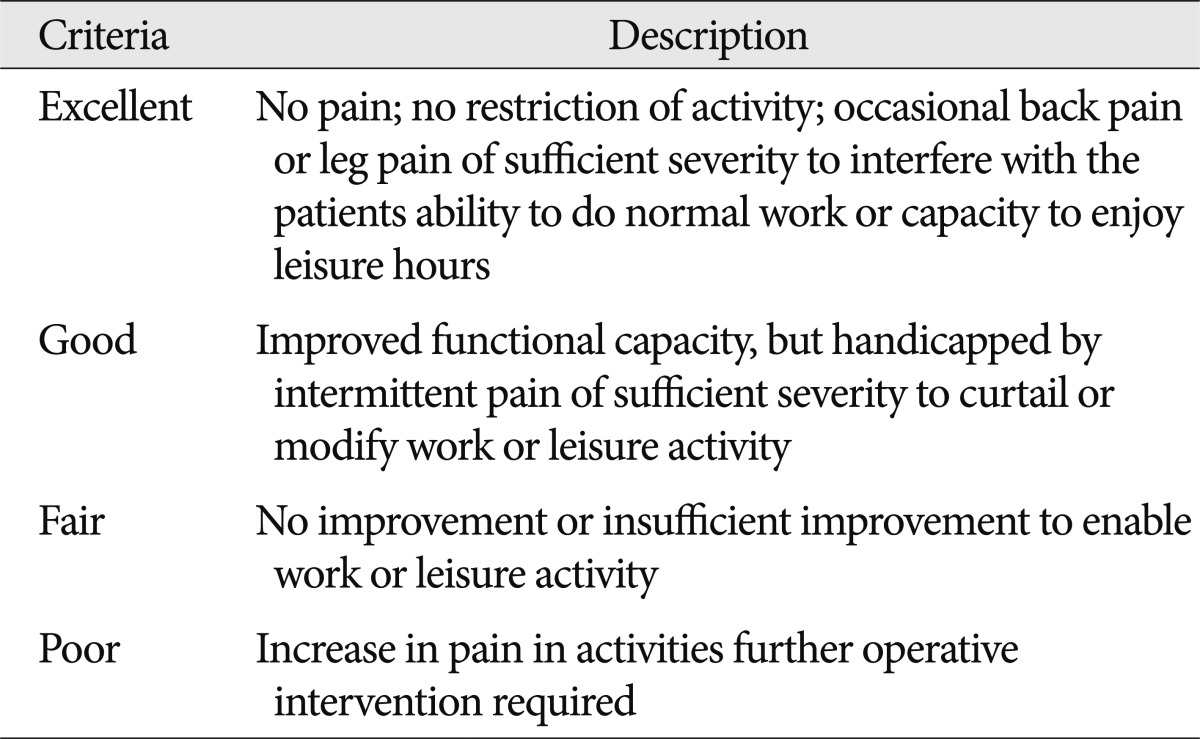
Table 3
Demographic and procedural details*
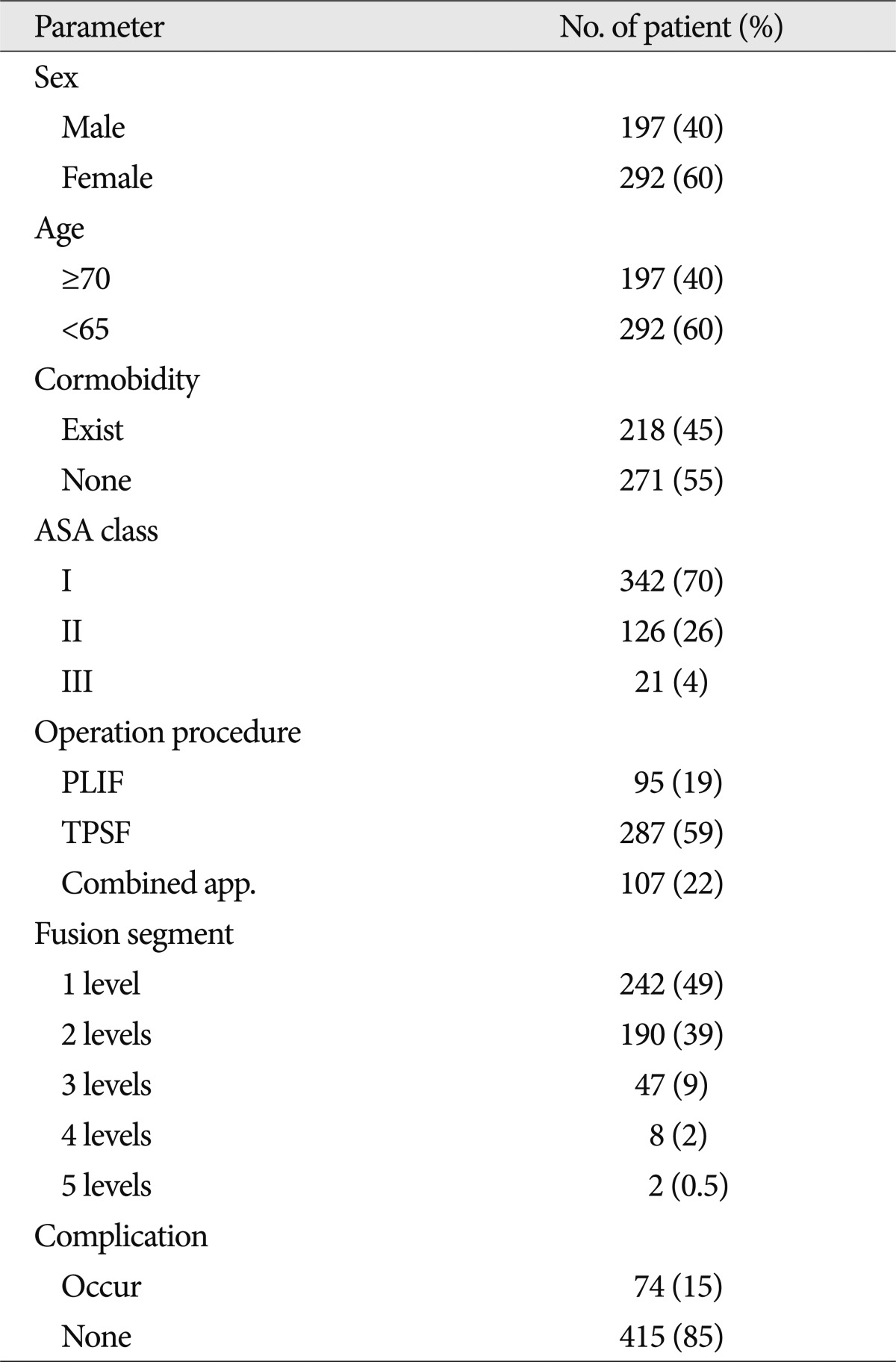
Table 4
Concomitant disease in 218 patients who underwent surgery for spinal fusion 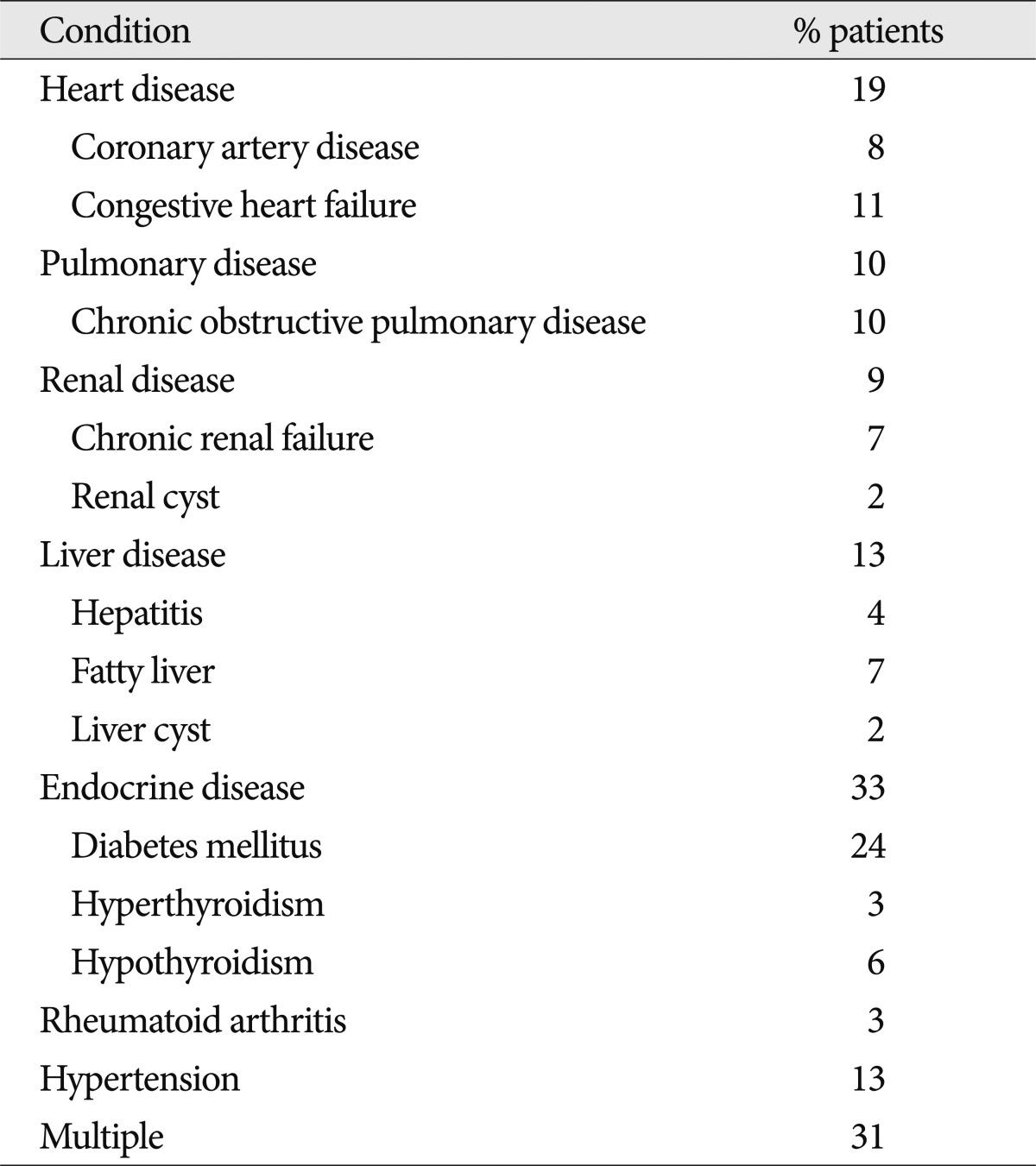
Table 5
Univariate analysis between age and concomitant disease*
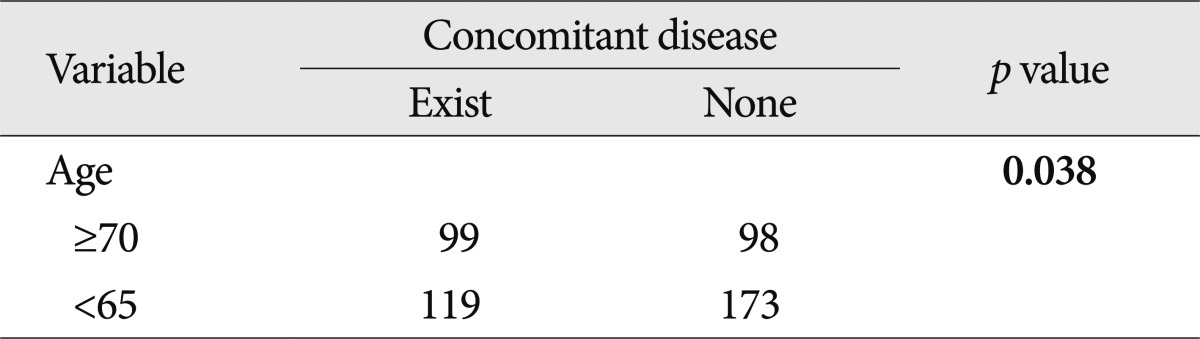
Table 6
Incidence of complications according to disease 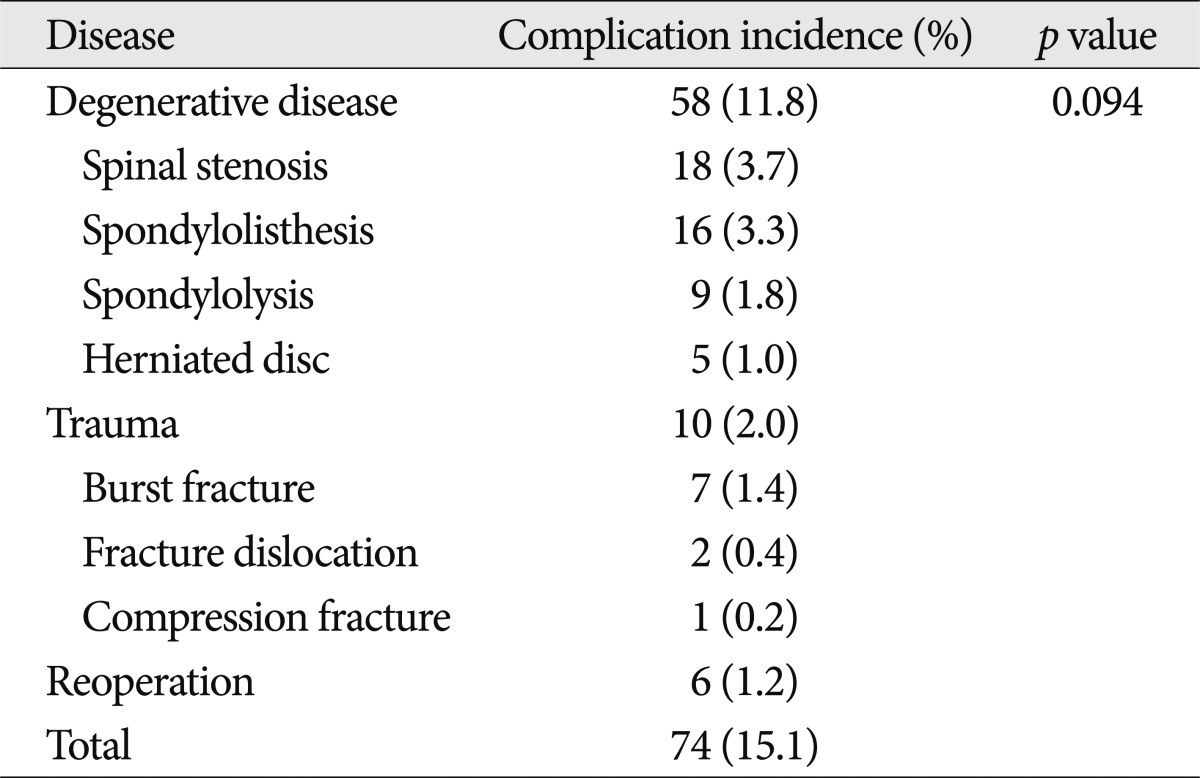
Table 7
Complications in 74 patients*
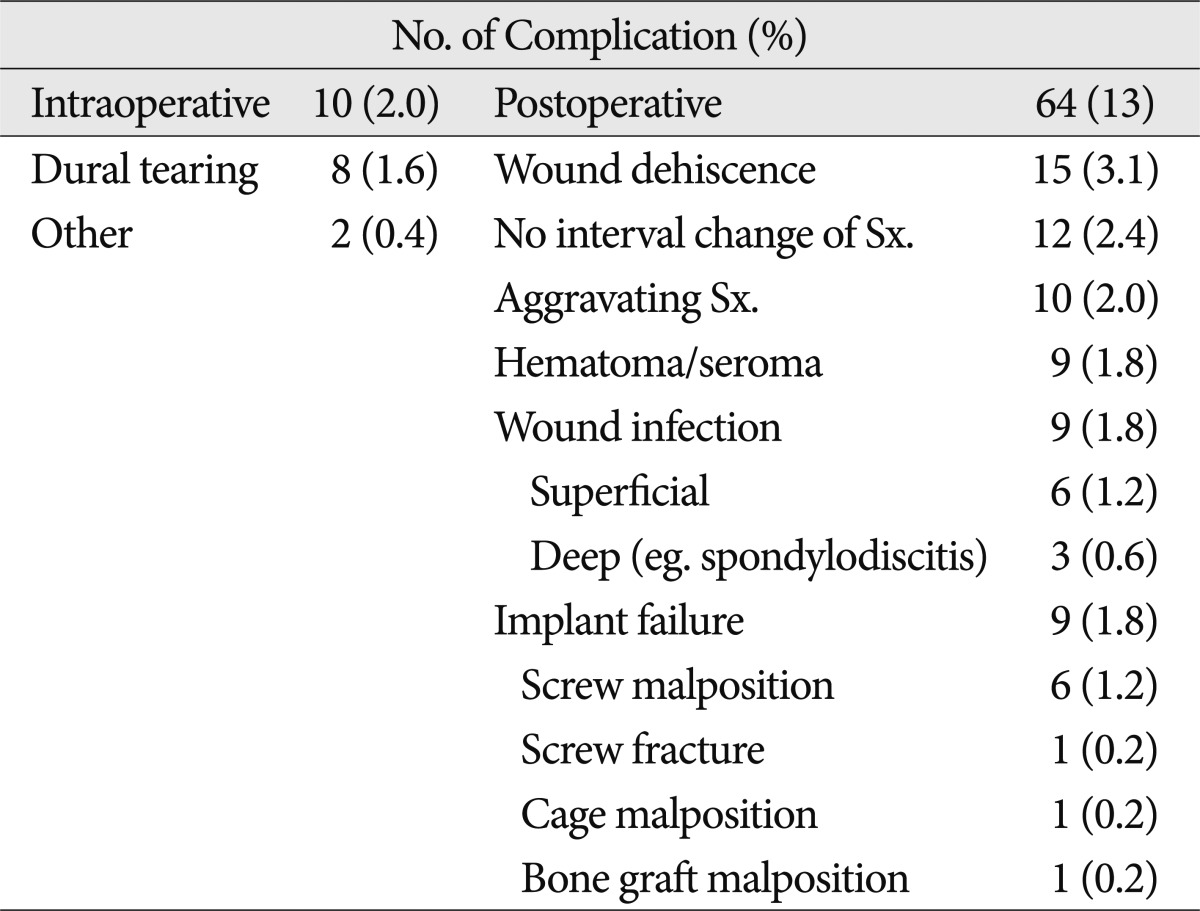
Table 8
Results of univariate and multivariate analysis*
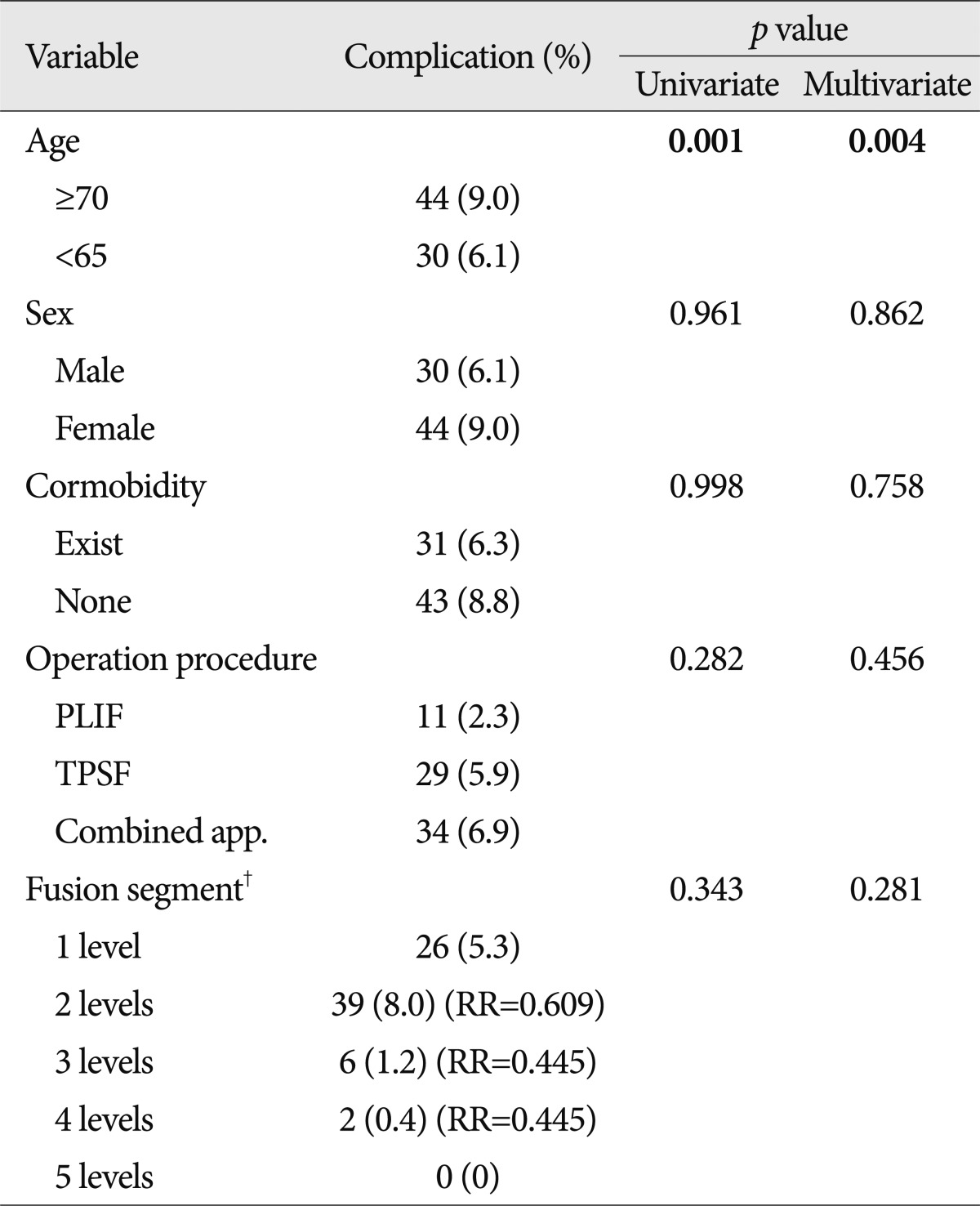
Table 9
Univariate analysis of age and sex related with bone mineral density*
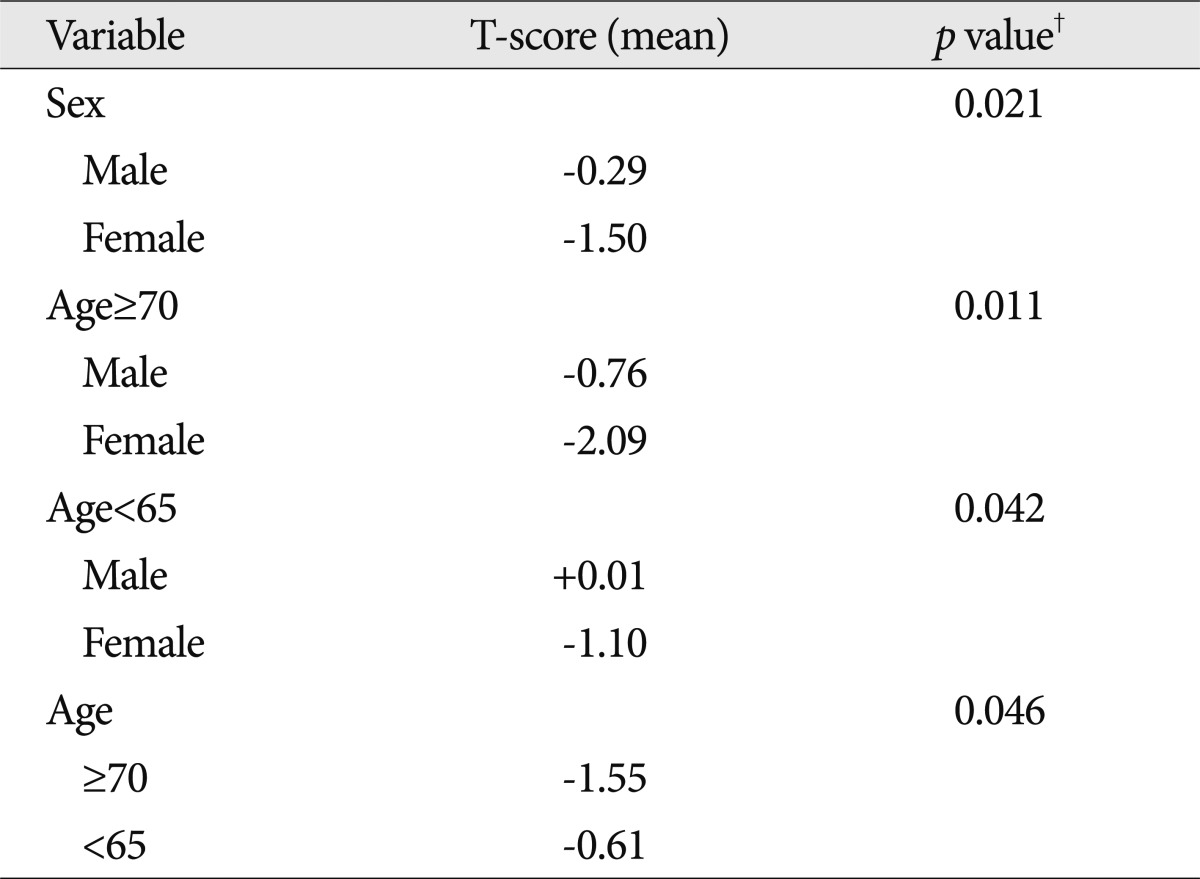
Table 10
Univariate analysis between bone mineral density and sex, age associated with complication*
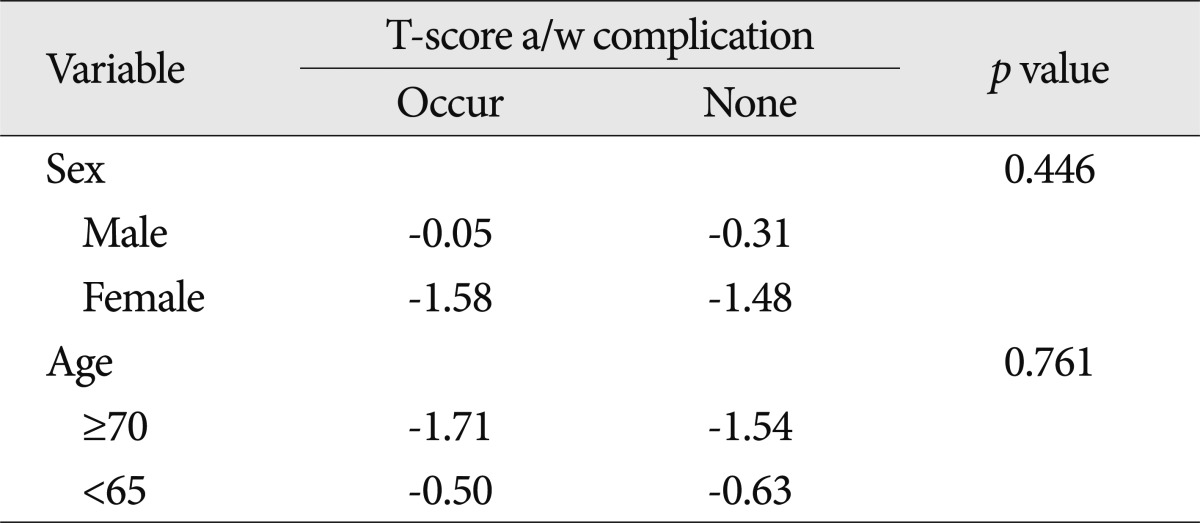
Table 11
Comparison of outcome according to age*
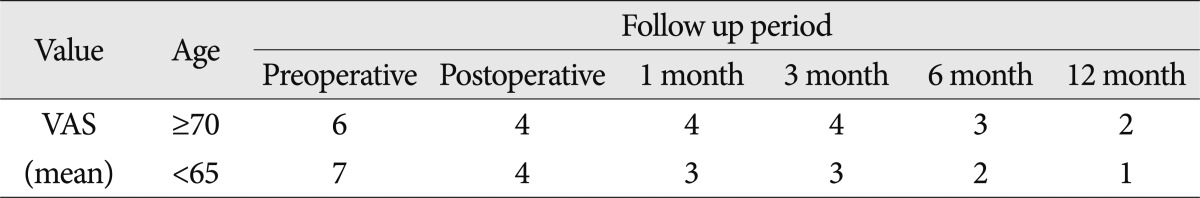
Table 12
Analysis of symptom improving according to complication*
|
|