Kim, Bak, Chun, Oh, Kang, and Yang: Posterior Interspinous Fusion Device for One-Level Fusion in Degenerative Lumbar Spine Disease : Comparison with Pedicle Screw Fixation - Preliminary Report of at Least One Year Follow Up
Abstract
Objective
Transpedicular screw fixation has some disadvantages such as postoperative back pain through wide muscle dissection, long operative time, and cephalad adjacent segmental degeneration (ASD). The purposes of this study are investigation and comparison of radiological and clinical results between interspinous fusion device (IFD) and pedicle screw.
Methods
From Jan. 2008 to Aug. 2009, 40 patients underwent spinal fusion with IFD combined with posterior lumbar interbody fusion (PLIF). In same study period, 36 patients underwent spinal fusion with pedicle screw fixation as control group. Dynamic lateral radiographs, visual analogue scale (VAS), and Korean version of the Oswestry disability index (K-ODI) scores were evaluated in both groups.
Results
The lumbar spine diseases in the IFD group were as followings; spinal stenosis in 26, degenerative spondylolisthesis in 12, and intervertebral disc herniation in 2. The mean follow up period was 14.24 months (range; 12 to 22 months) in the IFD group and 18.3 months (range; 12 to 28 months) in pedicle screw group. The mean VAS scores was preoperatively 7.16┬▒2.1 and 8.03┬▒2.3 in the IFD and pedicle screw groups, respectively, and improved postoperatively to 1.3┬▒2.9 and 1.2┬▒3.2 in 1-year follow ups (p<0.05). The K-ODI was decreased significantly in an equal amount in both groups one year postoperatively (p<0.05). The statistics revealed a higher incidence of ASD in pedicle screw group than the IFD group (p=0.029).
Conclusion
Posterior IFD has several advantages over the pedicle screw fixation in terms of skin incision, muscle dissection and short operative time and less intraoperative estimated blood loss. The IFD with PLIF may be a favorable technique to replace the pedicle screw fixation in selective case.
Key Words: Degenerative ┬Ę Fusion device ┬Ę Interspinous ┬Ę Lumbar disease ┬Ę Posterior ┬Ę Adjacent segmental degeneration.
INTRODUCTION
Transpedicular screw fixation has been the treatment of choice for stabilizing segmental instability and in cases which wide decompression is required. However, the use of pedicle screw is not suitable for all cases of degenerative spine disease. There are some disadvantages such as postoperative back pain resulted from wide muscle dissection and long operative times. It is also associated with increased rates of cerebrospinal fluid leakage, nerve injury, deep wound infection and hardware failure 5,9). Posterior fusion may alter the normal biomechanics of the spine, and a loss of motion at the fused levels may cause an increase in motion at adjacent segments 12,18). As a result, a significant amount of additional force will be placed on the facet joints at adjacent levels. One commonly observed consequence of fusing spinal motion segments is adjacent segmental degeneration (ASD) that is attributed to the increasing forces on adjacent levels 22). To reduce the risks associated with the pedicle screw fixation, interspinous fixation has been attempted. In the present study, we report the results of patients who underwent the interspinous fusion device (IFD) augmented with posterior lumbar interbody fusion (PLIF). The data acquired in these patients are compared with those obtained from patients who underwent pedicle screw fixation during the same period.
MATERIALS AND METHODS
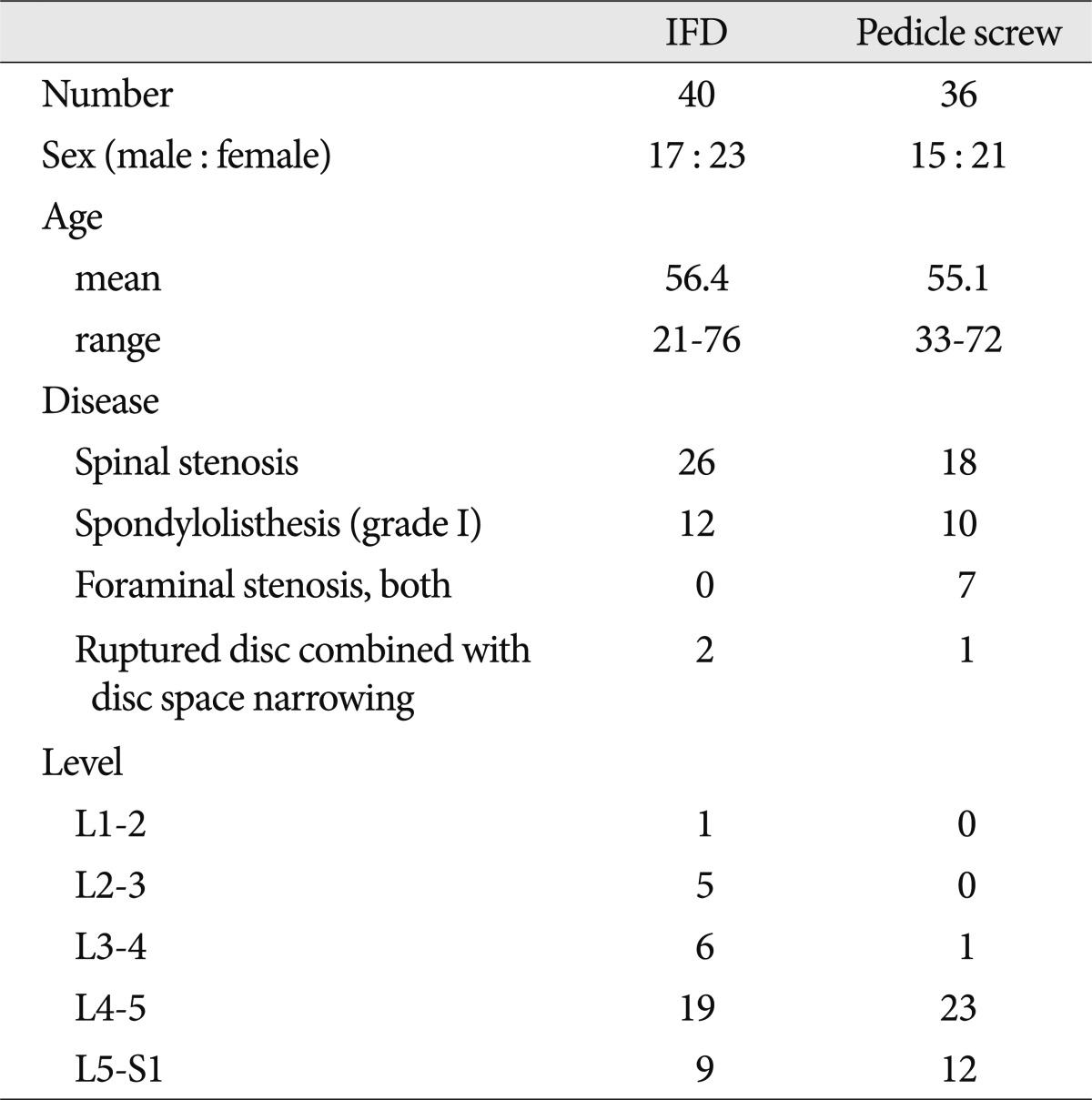
This study included a total of 76 adult patients with degenerative lumbar spinal diseases, who consecutively underwent posterior IFD (SPIRE┬«, Medtronic Sofamor Danek, Memphis, TN, USA) ( Fig. 1) or pedicle screw fixation between Jan. 2008 and Aug. 2009. The demographic data of the patients is listed on Table 1. The IFD group included 40 patients, 17 males and 23 females, who ranged in age from 21 to 76 years (mean 56.4 years) at the time of surgery. Lumbar spine diseases in the IFD group were as follows; spinal stenosis in 26 patients, degenerative spondylolisthesis (grade I) in 12 patients, and intervertebral disc herniation with severe intervertebral disc height loss in 2. In operated levels in the IFD group, L4-5 was most common (19 cases). Patients with advanced degenerative spondylolisthesis (Ōēźgrade II), spondylolysis, infection and lesions involving more than two levels were excluded. The patients who underwent transpedicular screw fixation (pedicle screw group) included 36 patients. There were 15 male and 21 female patients who ranged in age from 33 to 72 years (mean; 55.1 years). The mean follow up period was 14.24 months (range; 12 to 22 months) in the IFD group and 18.3 months (range; 12 to 28 months). Patients' charts were reviewed to collect data regarding estimated blood loss (EBL), operative time, and hospital length of stay (LOS) from the two groups, as well as to determine whether there were surgery-related complications.
Dynamic and static radiographs were evaluated at 1, 6, and 12 months postoperatively and reviewed by the authors and neuroradiologist. Lumbar computed tomography (CT) scan was checked 6 months after the surgery to check the fusion status quo. Bone fusion was defined as a presence of trabecular bone on the sagittal view of the lumbar CT or an angle change of less than 2 degrees in comparison with flexion and extension lateral radiographs 23). The segmental angle was measured with the angle formed by the lines drawn on the lower endplate of the upper lumbar body of the adjacent segment and the lines drawn on the upper endplate of the lower lumbar body using simple lateral X-ray (neutral, flexion, and extension) radiographs, and were compared between the angle on extension and that on flexion. The total sum of intervertebral angles between flexion and extension per level meant the range of motion (ROM) at that level. According to White and Panjabi's instability in the lumbar spine, we defined the potential instability if the segmental intervertebral angle change of L1-2, L2-3, L3-4 exceeds 15 degrees and that of L4-5 exceeds 20 degrees and that of L5-S1 exceeds 25 degrees between flexion and extension lateral radiographs. ASD was defined as a sagittal translation of the adjacent vertebral body above the fused level greater than 3 mm on the standing lateral film, and obvious segmental instability 15). The clinical outcome was measured using the visual analogue scale (VAS) score and the Korean version of the Oswestry disability index (K-ODI) score. Although randomly allocated, there were no significant differences in these scores preoperatively between two groups. Immediate postoperative follow up evaluation was checked on the day after surgery. All patients were evaluated at the outpatient clinic in regular intervals at 1, 6, and 12 months after surgery.
SPSS software with version 17.0 (SPSS Inc., Chicago, IL, USA) was used to statistically analyze all of the data. The Mann-Whitney U test, Wilcoxon signed ranks test, and Fisher's exact test were used based on the characteristics of the variables being compared. A probability value of less than 0.05 was the minimum value of statistical significance.
Operative procedure
Operative procedures were performed at only single level in our institute by one neurosurgeon. All patients in the IFD group and pedicle screw group underwent PLIF with a polyetheretherketone cage (PLIVIOS® cage, Synthes, Ontario, USA) or a titanium alloy cage (OTIS® cage, BK Meditech, Seoul, Korea). Pedicle screw fixation was achieved via standard open approach.
The IFD is composed of two titanium plates with aggressive, opposing spikes connected at their midpoint by a polyaxial stem. The IFD is inserted between the rostral and caudal portions of spinous processes, and each blades make maximal contact with their respective spinous processes 21). An approximately 4 cm midline skin incision was made overlying the spinous processes at the target level. After dividing the lumbodorsal fascia, electrocautery was used to perform a subperiosteal dissection to elevate the erector spinae muscles bilaterally off the rostral and caudal spinous processes down to the spinolaminar junction. The interspinous ligament at the target level was then removed with rongeurs. The supraspinous ligament of each spinous process was left in place to facilitate anatomical closure. Portions of the spinous processes and laminae may also be harvested for autograft and placed in the interspinous and laminar space for posterior arthrodesis prior to implanting the plate.
Care should be taken to ensure that no part of the plate protrudes above the lumbodorsal fascia. Once the two plates are situated optimally with one plate on either side of the spinous processes and the stem in the interspinous space, hand-held compression instruments are used to clamp the plates towards each other, driving the spikes into the bone. While compression is maintained, a locking screw is inserted and tightened to a predetermined torque. The top of the locking plug breaks away and rigid fixation is achieved. Lastly, a standard multi-layered closure is performed ( Fig. 2).
RESULTS
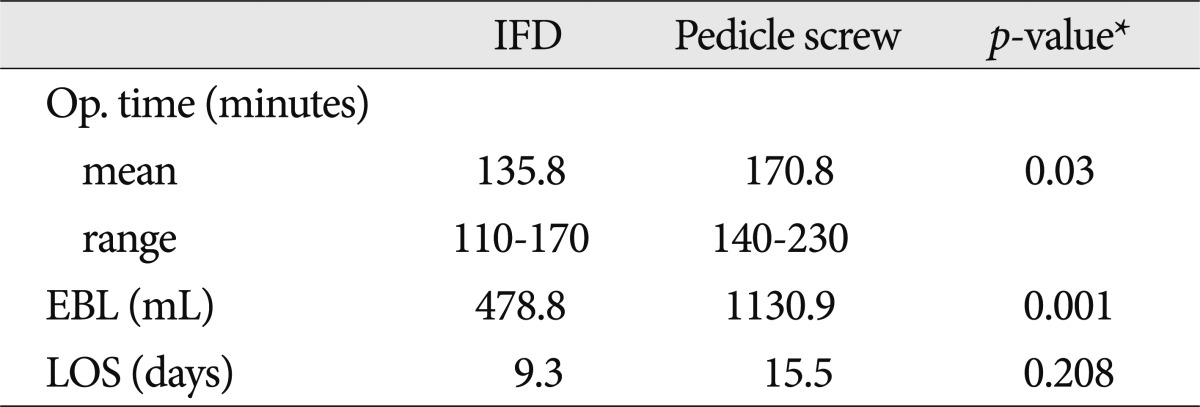
Operative outcome (Table 2)
There were no statistically significant differences in sex and age between the two groups. The mean operative time in the IFD group (135.8 minutes, range 110-170 minutes) was significantly less than that in pedicle screw group (170.8 minutes, range 140-230 minutes) (p=0.03). EBL was also significantly less (mean 478.8 mL, range 120-1000 mL) in the IFD group than in pedicle screw group (mean 1130.9 mL, range 500-1700 mL) (p=0.001). The mean LOS (including the day of surgery) was 9.3 days in the IFD group and 15.5 days in pedicle screw group, which was not statistically significant (p=0.208).
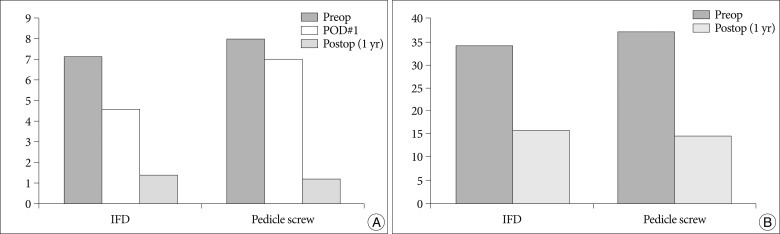
Clinical outcome assessment (Fig. 3)
The VAS score was recorded preoperatively 7.16┬▒2.1 and 8.03┬▒2.3 in the IFD group and pedicle screw group, respectively, and was improved postoperatively to 1.3┬▒2.9 and 1.2┬▒3.2 in the IFD group and pedicle screw group, respectively in 1-year follow ups (p<0.05). At immediate postoperative follow up (POD#1), VAS score was much improved to 4.6┬▒3.7 in the IFD group than 7.0┬▒3.5 in the pedicle screw group (p<0.05).
The K-ODI was reduced significantly in an equal amount in the patients of both groups in one year postoperatively (p<0.05). No statistical difference in clinical outcomes was noticed between the two groups.
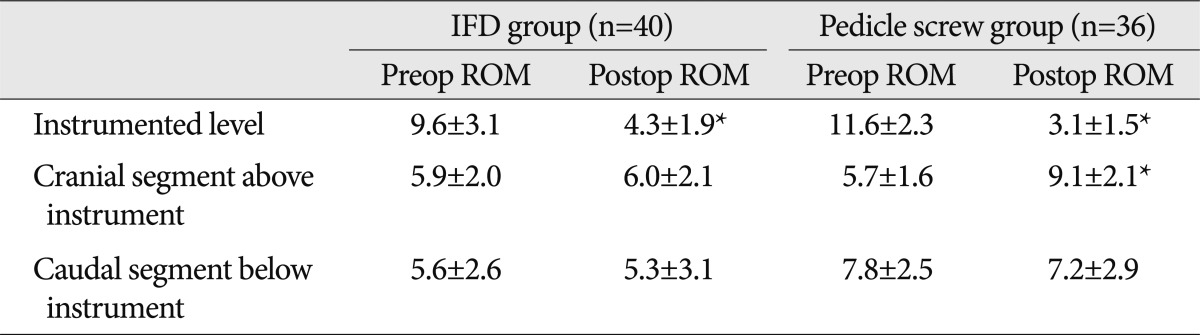
Radiological outcome assessment
There was no significant difference in the preoperative segmental intervertebral angle change at each level between two groups. The postoperative radiographs in pedicle screw group indicated that the ROM at the instrumented level (3.1┬▒1.5) was significantly decreased compared with the preoperative ROM (11.6┬▒2.3) ( p<0.05). In the IFD group, the postoperative ROM at the instrumented level (4.3┬▒1.9) was also decreased significantly compared with the preoperative ROM (9.6┬▒3.1) ( p<0.05), although the amount of decrease was not as much as observed in pedicle screw group ( Table 3). The ROM at the upper adjacent segment in the pedicle screw group was 5.7┬▒1.6 in pre-operation and 9.1┬▒2.1 in post-operation. It was increased significantly after surgery (p<0.05), while the ROM in the IFD group did not significantly postoperatively change at this level (p=0.66). The ROM at the lower adjacent segment was reported no statistically significant differences after surgery in both groups.
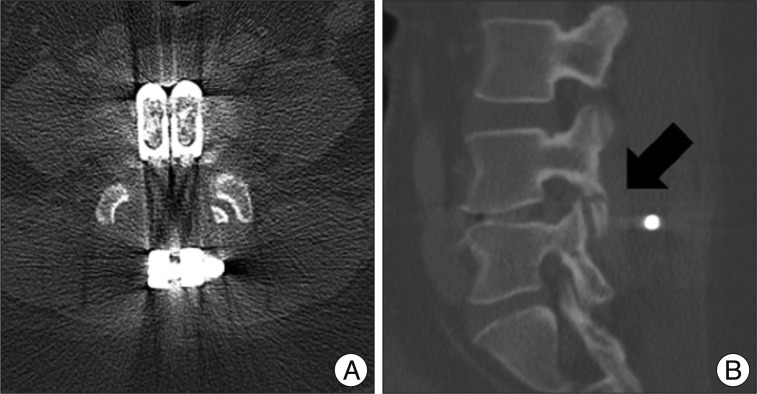
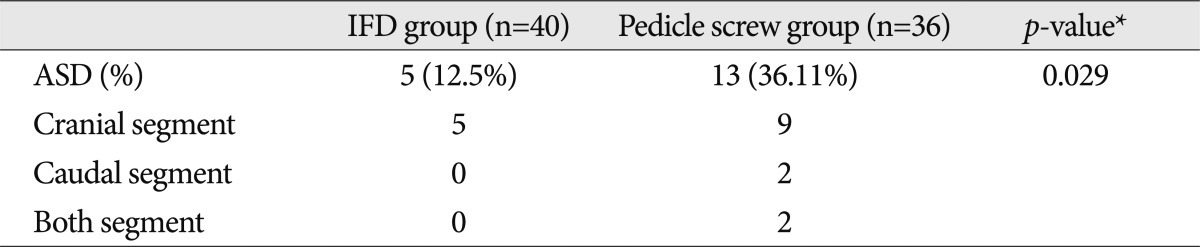
The number of patients with ASD was 5 (12.5%) in the IFD group and 13 (36.1%) in pedicle screw group. The Fisher's exact test revealed that the change in the segmental angle of the adjacent segment was much increased in pedicle screw group than the IFD group ( p=0.029) ( Table 4). In the IFD group, ASD was observed at cranial segment in all cases. Among 13 cases of ASD in pedicle screw group, 9 cases were reported in the cranial segment and 2 cases in the caudal segment. Of the 40 patients in the IFD group, bone fusion was observed in 37 patients (92.5%). Among 36 patients in pedicle screw group, bone fusion was noted in 33 patients (91.6%). In the IFD group, one patient had sustained back pain, and lumbar CT revealed fusion failure and fracture on L4 inferior articular process ( Fig. 4). Another two patients showed retropulsion of interbody cage on a follow up radiograph and required Re-operation. There were no major surgery-related complications such as deep infection, nerve root injury, and CSF leakage in the IFD group. However, of the 36 patients in pedicle screw group, deep infection in 3 cases, CSF leakage in 2 cases, and postoperative epidural hematoma required re-operation in 1 case were reported.
DISCUSSION
Spinal fusion is commonly performed in spine surgery to improve the pain and clinical outcomes of patients with failed conservative treatment for degenerative lumbosacral disease by reducing segmental instability, which is recognized as a major cause of low back pain. Currently, pedicle screw fixation or posterior interbody fusion is the gold standard for surgical management of lumbar spinal instability 1,22). It has proven to be effective, with reported lumbar fusion rates as high as 96% 4,6,19,23). However, lumbar fusion with instruments does not always lead to favorable results. Transpedicular fixation is associated with significant risks as followings; 4% cerebrospinal fluid leakage, 2% transient neurapraxia, 2% permanent nerve root injury, 4 to 5% deep tissue infection, and 3 to 12% hardware failure 5,9). Recently, numerous complications and problems after fusion surgery have been reported, with ASD being one of the most important. As a cause of ASD, Cunningham et al. 3) reported a significant increase in the intervertebral disc pressures by destabilization of the adjacent lumbar spine followed by stabilization with instrumentation. Still, the exact etiology is uncertain but alteration in facet loading, hypermobility, and increased intradiscal pressure at the segments adjacent to fusion mass is believed to play certain key roles 7,8,12,14,16). Spinal fusion alters the biomechanics of the spine and the loss of motion at the fused levels is at least theoretically compensated by increased motion at other unfused segments resulting in ASD 11). Superior segment facet violation or laminectomy has recently shown in vitro to destabilize the adjacent level in pedicle screw fixation 2). In contrary, a recent comparative biomechanical study showed that the IFD reduced the ROM and load on the disc and articular processes stresses, while it increased loads transmitted through the spinous processes 13). And the IFD can preserve normal anatomy and does not violate adjacent facet joints, making it less likely to cause hardware-related pain or to accelerate adjacent facet degeneration 20). In the present study, it tended to affect the adjacent segment less than a pedicle screw. A recent clinical study showed that the incidence of ASD in the cephalad adjacent segment 10 years following 360┬░ instrumented lumbar fusion averaged 21% 17). In the present study, the incidence of ASD was 36.1% in the patients who received pedicle screw fixation, significantly higher incidence compared with the IFD group in which it was 12.5% ( p=0.029). We showed that ROM at the instrumented level was significantly decreased in both the IFD and pedicle screw group compared with the preoperative state. This means that the IFD has some stabilizing effect at an unstable segment. Wang et al. 21) have studied the biomechanical characteristics of the IFD in an in vitro test of 109 cadaveric specimens and resulted that the greatest mean limitation of flexion-extension ROM was 4.14┬░ for IFD with lumbar interbody fusion whereas it was 5.03┬░ for pedicle screw fixation with lumbar interbody fusion, and 10.13┬░ for the intact spine. With an interbody device, the IFD provided the greatest limitation in flexion and extension over pedicle screw constructs. In short, the IFD provides enough segmental rigidity to make it a viable alternative to pedicle screw fixation. However, the IFD has some weak point which cannot effectively control the axial rotation and lateral bending. Recent paper by Karahalios et al. 10) demonstrated, through cadaveric study, that the capacity controlling ROM such as axial rotation and lateral bending is lack compared with transpedicular screw fixation when only interspinous device used as following; ROM of lateral bending was -3.83┬▒1.47 in left and 3.92┬▒1.26 in case used only interspinous device. These ROM was superior to normal motion, but inferior to transpedicular screw fixation (ROM of lateral bending was -0.57┬▒0.14 in left and 0.57┬▒0.09). However, their papers revealed that lumbar interbody fusion gave the control of ROM to the IFD. Via cadaveric study, there was no statistically significant difference of ROM between IFD with lumbar interbody fusion and pedicle screw fixation with lumbar interbody fusion. Also, the IFD implant have several advantage compared with pedicle screw. It is less invasive and presents no risk of dural or neural injury and cerebrospinal fluid leakage because it is placed on only the spinous process. In addition to the easy maneuverability of the IFD implantation, the operative time for cases involving the IFD was shorter than that for cases involving pedicle screw fixation. Less time in the operating room also leads to reduced hospital and healthcare costs. Similarly, intraoperative EBL was much less in cases involving the IFD; it was 50% lower than that in patients who underwent open pedicle screw fixation. The minimal bone exposure, easy implantation, and short operative time required for implantation will contribute to decreasing EBL. Because many patients undergoing lumbar fusion are elderly, a lower EBL may help prevent anemia and other postoperative complications. Additionally, the IFD needs a smaller incision and requires less muscle and soft tissue retraction than the pedicle screw fixation. So, it may lead to less postoperative discomfort and we showed that immediate postoperative VAS scores in the IFD group were much lower than pedicle screw group in this study.
Although postoperative radiographs in the IFD group showed less improvement of instability at the instrumented level compared with in pedicle screw group, patients showed a similar clinical improvement as represented by K-ODI, and VAS scores. If more long-term studies confirm this clinical outcome, such techniques that preserve much of normal anatomy and biomechanical function of the lumbar spine as interspinous implant, will be highly indicated in the surgical treatment of spinal stenosis with various instability. It is attractive to alter the pedicle screw fixation for selected patients requiring instrumentation augmented fixation. In particular, the IFD may be well suited implant for augmenting the lumbar interbody fusion.
It is important to note that the application of the IFD is contraindicated in patients with pars interarticularis defects or any incompetence in the bone between anterior and posterior spinal columns 21). In addition, patients with advanced degenerative spondylolisthesis (Ōēźgrade II) are not good candidates for interspinous fixation. This study has some limitations. As a retrospective unrandomized design, it couldn't exclude all the factors that affect the results. And, because the incidence of ASD was investigated during short period of follow up, ASD was likely to occur after follow up period. So, a prospective, randomized trial with long-term follow up period is needed to confirm the efficacy of the SPIRE┬« plate as IFD.
CONCLUSION
Although the IFD is placed only on the spinous process, it provides immediate rigid fixation of the destabilized motion segments with interbody fusion that is comparable to the pedicle screws. The plate also does not violate adjacent facet joints, making it less likely to cause ASD. The IFD with PLIF may be an alternative technique if commanded under selective case.
References
1. Bridwell KH, Sedgewick TA, O'Brien MF, Lenke LG, Baldus C : The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 1993, 6 : 461-472,   2. Cardoso MJ, Dmitriev AE, Helgeson M, Lehman RA, Kuklo TR, Rosner MK : Does superior-segment facet violation or laminectomy destabilize the adjacent level in lumbar transpedicular fixation? An in vitro human cadaveric assessment. Spine (Phila Pa 1976) 2008, 33 : 2868-2873,   3. Cunningham BW, Kotani Y, McNulty PS, Cappuccino A, McAfee PC : The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure : an in vitro biomechanical analysis. Spine (Phila Pa 1976) 1997, 22 : 2655-2663,   4. Dickman CA, Fessler RG, MacMillan M, Haid RW : Transpedicular screw-rod fixation of the lumbar spine : operative technique and outcome in 104 cases. J Neurosurg 1992, 77 : 860-870,   5. Esses SI, Sachs BL, Dreyzin V : Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976) 1993, 18 : 2231-2238; discussion 2238-9,   6. Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT : 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis : a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976) 1997, 22 : 2807-2812,   7. Ghiselli G, Wang JC, Hsu WK, Dawson EG : L5-S1 segment survivorship and clinical outcome analysis after L4-L5 isolated fusion. Spine (Phila Pa 1976) 2003, 28 : 1275-1280; discussion 1280,   8. Hilibrand AS, Robbins M : Adjacent segment degeneration and adjacent segment disease : the consequences of spinal fusion? Spine J 2004, 4 : 190S-194S,   9. Jutte PC, Castelein RM : Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J 2002, 11 : 594-598,   10. Karahalios DG, Kaibara T, Porter RW, Kakarla UK, Reyes PM, Baaj AA, et al : Biomechanics of a lumbar interspinous anchor with anterior lumbar interbody fusion. J Neurosurg Spine 2010, 12 : 372-380,   11. Lafage V, Gangnet N, S├®n├®gas J, Lavaste F, Skalli W : New interspinous implant evaluation using an in vitro biomechanical study combined with a finite-element analysis. Spine (Phila Pa 1976) 2007, 32 : 1706-1713,   12. Lee CK, Langrana NA : Lumbosacral spinal fusion. A biomechanical study. Spine (Phila Pa 1976) 1984, 9 : 574-581,   13. Papp T, Porter RW, Aspden RM, Shepperd JA : An in vitro study of the biomechanical effects of flexible stabilization on the lumbar spine. Spine (Phila Pa 1976) 1997, 22 : 151-155,   14. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE : Adjacent segment disease after lumbar or lumbosacral fusion : review of the literature. Spine (Phila Pa 1976) 2004, 29 : 1938-1944,   15. Schlegel JD, Smith JA, Schleusener RL : Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine (Phila Pa 1976) 1996, 21 : 970-981,   16. Schnake KJ, Schaeren S, Jeanneret B : Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976) 2006, 31 : 442-449,   17. Schulte TL, Leistra F, Bullmann V, Osada N, Vieth V, Marquardt B, et al : Disc height reduction in adjacent segments and clinical outcome 10 years after lumbar 360 degrees fusion. Eur Spine J 2007, 16 : 2152-2158,    18. Sonntag VK, Marciano FF : Role of spinal instrumentation in fusion for degenerative disease of the lumbosacral spine. West J Med 1995, 162 : 262-263,   19. Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, B├╝nger CE : 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion : a prospective, randomized clinical study. Spine (Phila Pa 1976) 1997, 22 : 2813-2822,   20. Wang JC, Haid RW Jr, Miller JS, Robinson JC : Comparison of CD HORIZON SPIRE spinous process plate stabilization and pedicle screw fixation after anterior lumbar interbody fusion. Invited submission from the Joint Section Meeting On Disorders of the Spine and Peripheral Nerves, March 2005. J Neurosurg Spine 2006, 4 : 132-136,   21. Wang JC, Spenciner D, Robinson JC : SPIRE spinous process stabilization plate : biomechanical evaluation of a novel technology. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2005. J Neurosurg Spine 2006, 4 : 160-164,   22. West JL 3rd, Ogilvie JW, Bradford DS : Complications of the variable screw plate pedicle screw fixation. Spine (Phila Pa 1976) 1991, 16 : 576-579,   23. Zdeblick TA : A prospective, randomized study of lumbar fusion. Preliminary results. Spine (Phila Pa 1976) 1993, 18 : 983-991,  
Fig.┬Ā1
A photograph shows the SPIRE® plate as a posterior interspinous fusion device. 
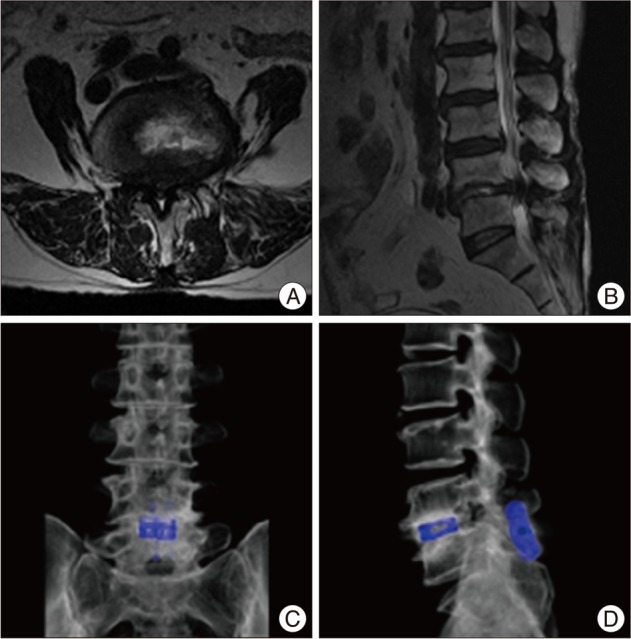
Fig.┬Ā2
A representative case of a patient with interspinous fusion device. Preoperative axial (A) and sagittal (B) magnetic resonance imaging shows a degenerative lumbar spinal stenosis at L4-5. Postoperative 3-dimensional reconstructed tomographic images (C and D) shows posterior lumbar interbody fusion augmented with the interspinous fusion device. 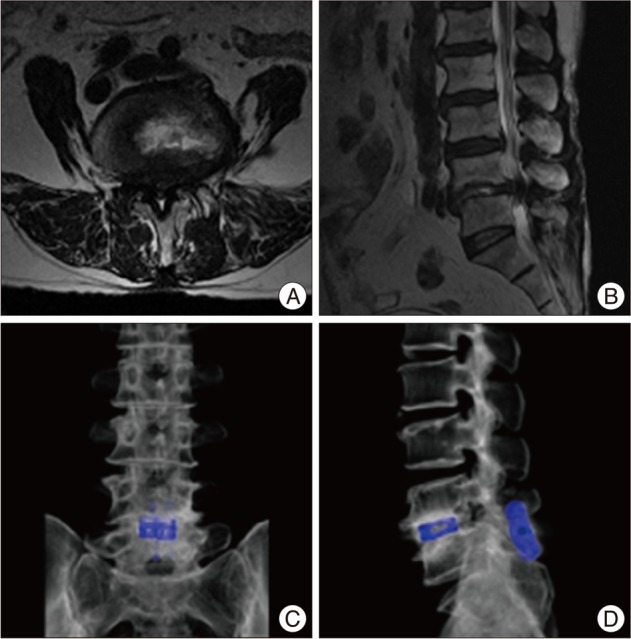
Fig.┬Ā3
Graph shows improvement of clinical outcome both in the interspinous fusion device group and pedicle screw group after surgery (p<0.05). A : Visual analogue scale score. B : Korean version of the Oswestry disability index. Preop : preoperation, Postop : postoperation, IFD : interspinous fusion device. 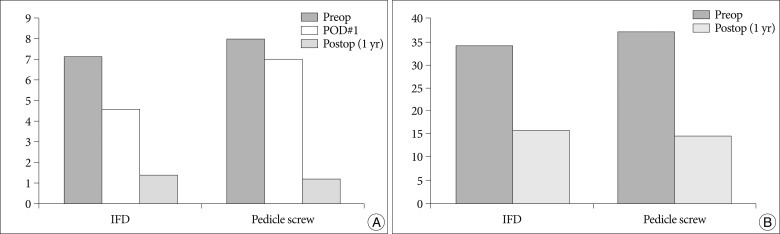
Fig.┬Ā4
A case of fusion failure and the fracture of articular process after interspinous fusion. Axial (A) and sagittal (B) view of the computed tomography shows the fracture on L4 inferior articular process (black arrow). 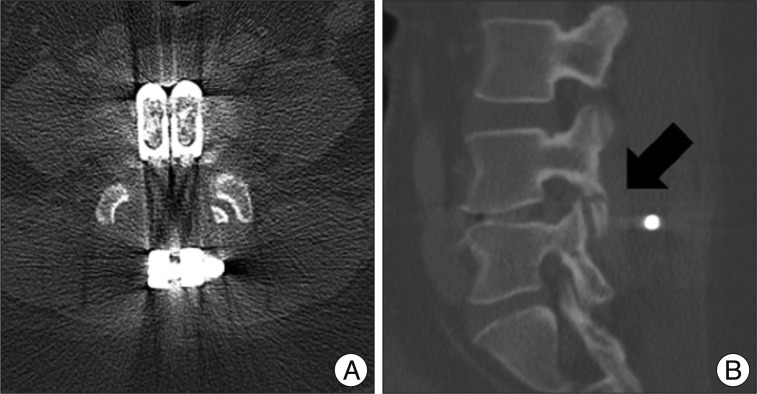
Table┬Ā1
Demographic data with specific spinal disorders in patients undergoing PLIF with IFD or pedicle screw fixation 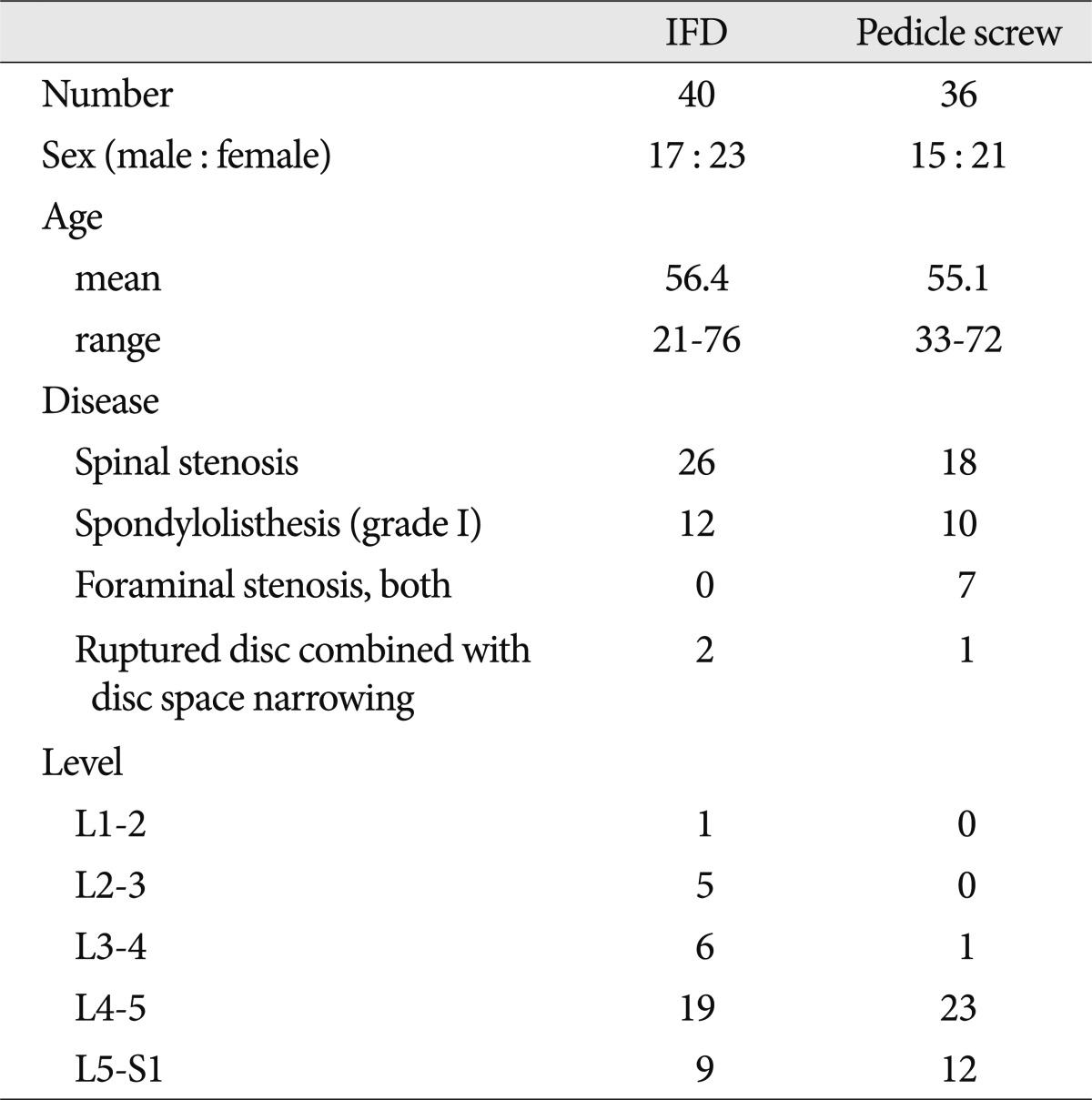
Table┬Ā2
Operative outcome of patients using either IFD or pedicle screw 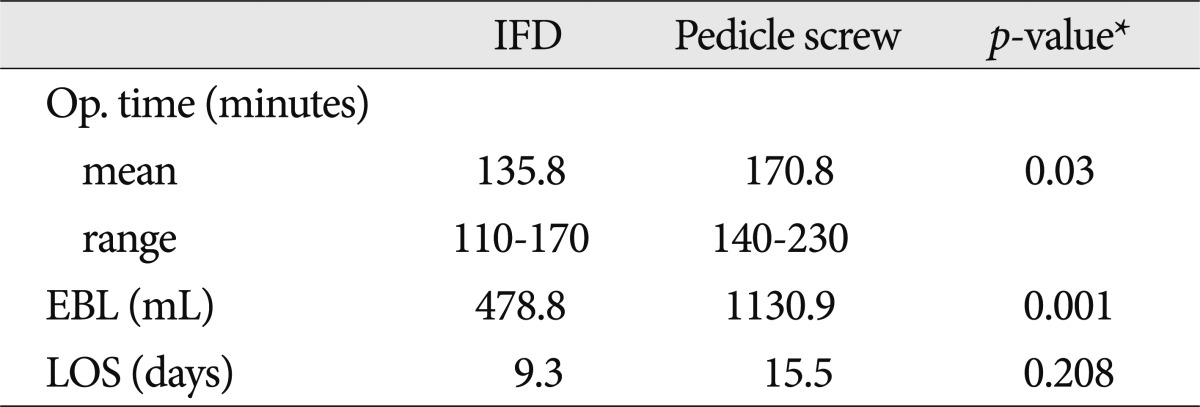
Table┬Ā3
Preoperative and postoperative 1-year follow up results of range of motion (ROM) at the instrumented and adjacent segments (Wilcoxon signed ranks test) 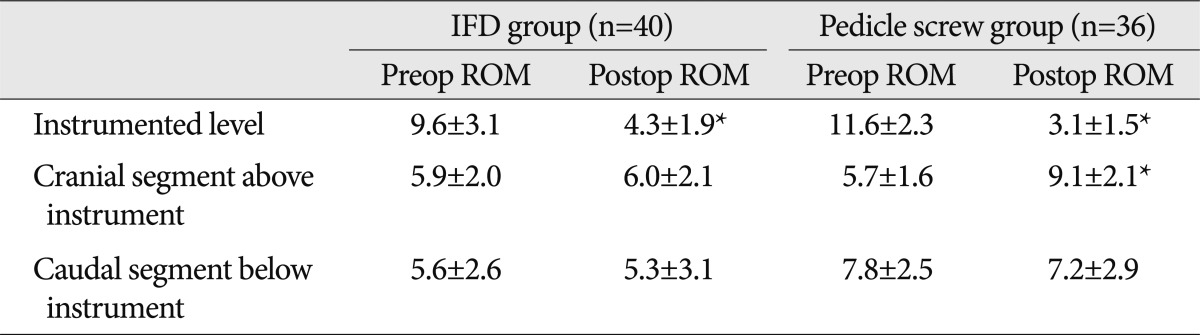
Table┬Ā4
Summary of adjacent segment disease emergence in the IFD group and pedicle screw group 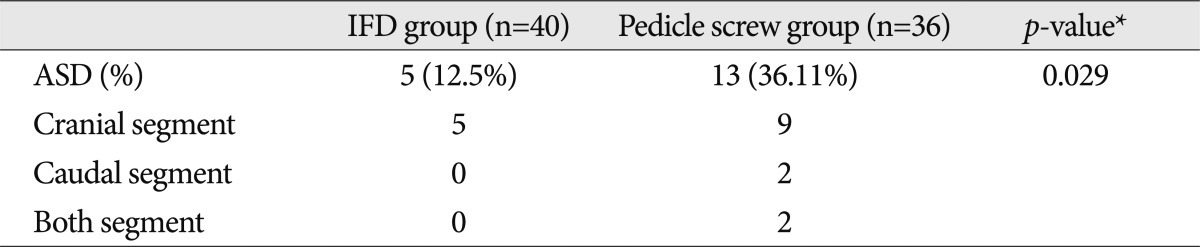
|
|