INTRODUCTION
Intradural lumbar disc herniation (ILDH) is a rare condition, having a reported incidence of 0.04-0.33% of all lumbar disc herniations12,20). Since Dandy first described it in 19425), the occasional reports of ILDH have rarely described the condition at above the L2-3 level12,16,17). Moreover, only one case of intradural cranial migration of disc materials has been described18).
Though ILDH can be diagnosed by means of magnetic resonance imaging (MRI), computed tomography (CT), and post-myelogram CT, such cases are rarely reported, due to physicians' limited experience with this condition and its nonspecific presentation16). In addition, in cases having either intradural disc fragments that migrated upward or downward or no direct connection between the protruded disc materials and intradural lesions, confusion with other spinal abnormalities, such as neurofibroma, lipoma, meningioma, epidermoid tumor, arachnoid cyst, or metastasis, may occur1,12).
In this report, we present a case of a sequestrated lumbar disc fragment which is upward migration in intradural space at the L2 vertebra level mimicking an intradural extramedullary (IDEM) spinal tumor.
CASE REPORT
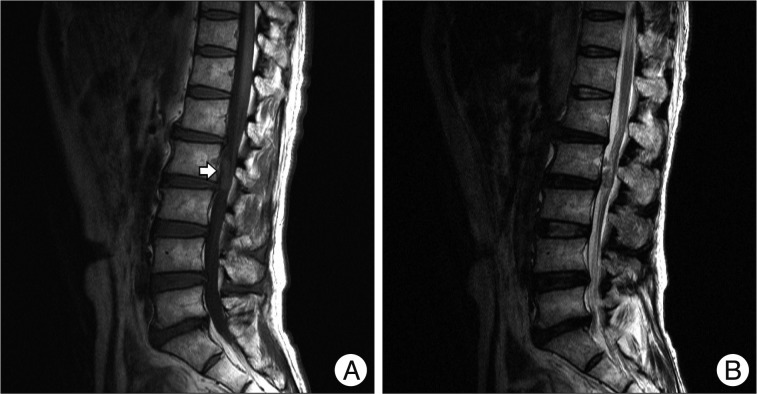
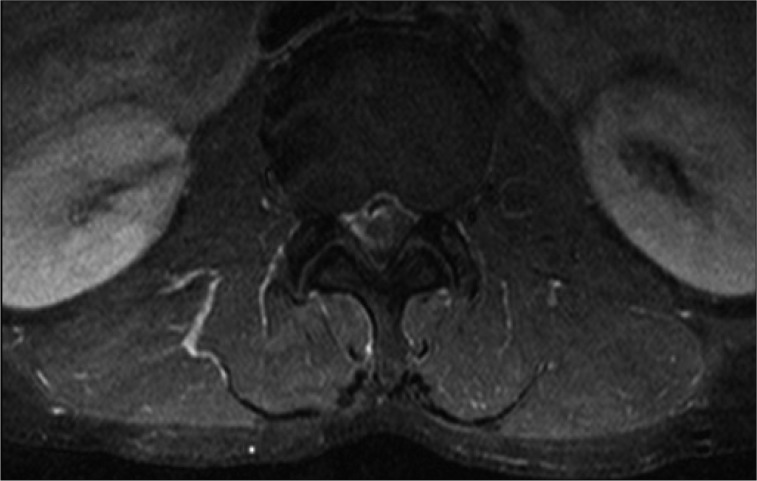
A 54-year-old man was admitted to the hospital after experiencing pain in his lower back and right leg for the preceding 2 months. His symptoms included a sudden exacerbation of pain for the 2 days prior to his admission. Neurologic examination revealed a positive straight leg raise test on his right side, without sensory, motor, or sphincter disturbances. An MRI showed an intradural mass-like lesion at the L2 level vertebral body and extending to the L2-L3 disc space, 10├Ś23 mm in size, with degenerative, diffuse disc bulging at all lumbar vertebral levels. This mass-like lesion had inhomogeneous signal intensity on a non-contrast MRI (Fig. 1). A gadolinium-enhanced MRI showed a partially-enhanced IDEM mass causing anterolateral compression of the nerve roots in the thecal sac (Fig. 2). The patient underwent surgical removal of the L2 and L3 laminae. Upon exploring carefully, we observed a swollen dural sheath, with dense external adhesions between the ventral dura and posterior longitudinal ligament (PLL). However, not only the dural sheath but also annulus of L2/3 intervertebral disc and PLL had no apparent defects or tearing.
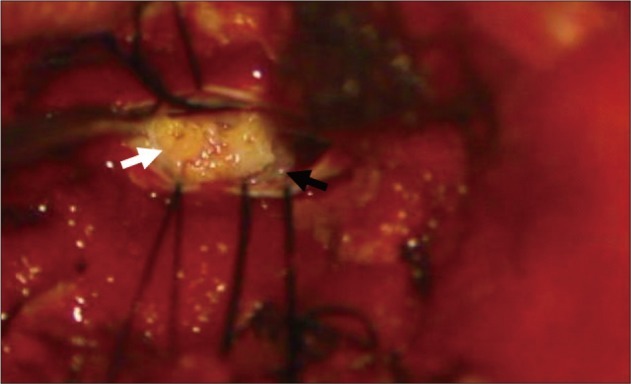
Upon making a longitudinal incision in the dura, we detected a 1├Ś2 cm, yellowish mass occupying the thecal sac, with peripheral displacement of the nerve roots (Fig. 3). Moreover, superior portion of the mass contacted the conus medullaris.
After carefully microdissecting the mass from the surrounding nerve roots and inner aspect of the ventral dura, the mass was totally removed. Although the ventral dura showed a dense adhesion to the PLL, no dural defects or tearing existed at the level of the mass. We sent a section of the mass for a frozen section biopsy, which ultimately confirmed it comprised degenerative nucleus pulposus, without any cellular elements. The surgery concluded upon primary closure of the durotomy site. The patient had no complication and his pain resolved significantly. He was discharged 1 week after the operation.
DISCUSSION
Intradural herniation of an intervertebral disc is a rare clinical entity, generally detected during surgery, and 92% of such intradural disc herniations (IDHs) are seen at the lumbar level9,17). ILDH's reported incidence is 0.04-0.33% of all lumbar disc herniations9,12,16). The most commonly affected site is L4-5 (55%), followed by L3-4 (16%) and then L5-S1 (10%)8,17). Although some authors, including Han et al.9), have reported ILDHs at the L2-3 level, such are quite rare. Moreover, intradural migration of disc fragment, to the level of the vertebral body from the level of ruptured intervertebral disc space, is particularly rare.
Although researchers are not certain of IDH's disease mechanism, the most widely accepted hypothesis states that adhesion between the ventral dura and PLL leads to the subsequent perforation of these firmly adhesive tissues, including the annulus fibrosus, due to the increased intradiscal pressure5,10,11,13). Floeth and Herdmann7) have reported that the herniated fragments work like a fingertip and the relative movements of the lumbar spine lead to a repetitive impression of the fixed dural sac and subsequent to a chronic inflammation and erosion process with thinning of the dura. Finally, the ligament and the adherent dura sheets are perforated and free disc material can herniate into the dural sac. Furthermore, some studies suggest that dense adhesions, whether congenitally formed or caused by trauma, previous surgery, inflammation, or osteophyte or disc protrusion, fixate the dural sac3,6,15). Many previous studies report seeing ILDH most frequently at the L4-5 level; the fact that the L4-5 level shows the densest adhesions between the PLL and ventral dura supports the hypothesis8,14,17).
ILDH's clinical symptoms generally include long-lasting low back pain and signs of cauda equina syndrome12,17). ILDH above the conus medullaris seems to lead to neurological dysfunction more rapidly than does ILDH below the conus medullaris. However, cases may present solely with signs of root compression17).
Myelography and myelo-computed tomography can accurately reveal this pathology, typically showing a complete blockage of the contrast medium, but these imaging methods do not allow the physician to characterize the compression's nature18,19). Although CT can provide valuable information, it cannot reliably identify intradural disc ruptures4). Benyamin et al.2) report an incidental diagnosis of ILDH that occurred during a discography. In that case, the physicians saw the annular fissure and extrusion of the injected contrast medium into the intrathecal space on the discography.
MRI is regarded as the most reliable method for diagnosing ILDH, and indeed for diagnosing any IDH. A study by Choi et al.4) presented a T2-weighted image showing the PLL's loss of continuity and its sharp, beak-like appearance, which presages an IDH. Wassestrom et al.21) reported an IDH with a rim enhancement pattern visible on a gadolinium-enhanced MRI. In spite of these diagnostic modalities for ILDH, the preoperative diagnosis of ILDH is difficult due to gadolinium-enhanced MRI being in limited use and to ILDH's rarity and nonspecific presentation9,16). In our case, we also observed a peripheral rim enhancement pattern on the gadolinium-enhanced MRI, but it depicted only a small, inferior portion of the mass.
Mut et al.15) classified IDH into types A and B. Type A is disc herniation into the dural sac, while type B is disc herniation into the dural sheath, in the preganglionic region of the nerve root. However, classifying IDHs into type A or B presents difficulties, not only because ILDH detection most often occurs incidental to other surgery, but also because Mut et al.15) based their classification on operative field findings2,17).
In our case, we located an intradural mass-like lesion at the level of the L2 vertebral body and extending into the L2-L3 disc space. Because most of the mass was at the level of the L2 vertebral body and totally within the thecal sac, we thought the mass might be an intradural extramedullary spinal tumor, such as a neurinoma, meningioma, ependymoma, or dermoid. Interestingly, however, biopsy revealed the mass to be an ILDH.
While Sarli├©ve et al.17) reported the first case of an intradural cranial migration of disc material, the patient in their case had undergone previous spinal surgery. Therefore, that patient had fibrosis and cicatricial arachnoiditis around the dura mater. In our case, the patient peculiarly had no history of trauma, previous surgery, or inflammation in the area. Moreover, he lacked any dural defect comprised of a dense adhesion between the ventral dura and PLL. Therefore, until biopsy revealed the mass was an ILDH, we could not have imagined that the mass was an intradural migration of sequestrated disc material.
CONCLUSION
We report a rare case of an ILDH that migrated upwardly from the level of the disc space to the level of vertebral body. In the treatment of a spinal intradural mass lesion, physicians should keep in mind the possibility of not only spinal tumors but also intradural disc herniation, to insure a correct diagnosis and proper management.