Park, Hwang, Jin, Bang, Oh, and Kwon: Intra-Arterial Thrombolysis Using Double Devices: Mechanicomechanical or Chemicomechanical Techniques
Abstract
Objective
To optimize the recanalization of acute cerebral stroke that were not effectively resolved by conventional intraarterial thrombolysis (IAT), we designed a double device technique to allow for rapid and effective reopening. In this article, we describe the feasibility and efficacy of this technique.
Methods
From January 2008 to September 2009, twenty patients with acute cerebral arterial occlusion (middle cerebral artery : n=12; internal carotid artery terminus : n=5; basilar artery : n=3) were treated by the double device technique. This technique was applied when conventional thrombolytic methods using drug, microwires, microcatheters and balloons did not result in recanalization. In the double device technique, two devices are simultaneously placed at the lesion (for example, one microcatheter and one balloon or two microcatheters). Chemicomechanical or mechanicomechanical thrombolysis was performed simultaneously using various combinations of two devices. Recanalization rates, procedural time, complications, and clinical outcomes were analyzed.
Results
The initial median National Institute of Health Stroke Scale (NIHSS) was 16 (range 5-26). The double device technique was applied after conventional IAT methods failed. Recanalization was achieved in 18 patients (90%). Among them, 55% (11 cases) were complete (thrombolysis in cerebral infarction 2B, 3). The median thrombolytic procedural time including the conventional technique was 135┬▒83.7 minutes (range 75-427). Major symptomatic hemorrhages (neurological deterioration Ōēź4 points in NIHSS) developed in two patients (10%). Good long term outcomes (modified Rankin Scale Ōēż2 at 90 days) occurred in 25% (n=5) of the cases. Mortality within 90 days developed in two cases (10%).
Conclusion
The double device technique is a feasible and effective technical option for large vessel occlusion refractory to conventional thrombolysis.
Key Words: Acute ┬Ę Stroke ┬Ę Thrombolysis ┬Ę Double devices.
INTRODUCTION
Recanalization of large cerebral artery occlusions by intraarterial thrombolysis (IAT) is difficult and conventional techniques using local thrombolytic drug infusion often fail 4,12). In our practice, chemical thrombolysis alone is rarely successful. Therefore, for many cases, mechanical methods are frequently applied for patients with large cerebral artery occlusions. Whether combined with other methods or done alone, mechanical methods that use wires, balloons and stents have produced better results in terms of high recanalization rates and few hemorrhagic complications 6,7,10,11). However, in many of our cases, a single mechanical technique using a single device has not often been enough to reopen the occluded vessels. Therefore, we have used several kinds of mechanical thrombolytic devices, such as wires, balloons and stents, alternatively in our practice. The choice of device was made so that the least traumatic device was used before those that are more traumatic. Thus, we had to withdraw devices from time to time in order to introduce another mechanical device or to infuse thrombolytic agents locally. In our experience, exchanging devices during IAT was troublesome and in many cases, technically difficult, time consuming and risky. To overcome these difficulties, we designed a double device technique in which we place two devices at the lesion through one large bore guiding catheter. The combination of the two devices varies (e.g., a microcatheter and other mechanical device such as a microwire, balloon, soft coil or stent or two different mechanical thrombolytic devices). While the mechanical thrombolysis is performed, thrombolytic agents are infused simultaneously through the microcatheter, a selective angiogram is obtained, or another mechanical thrombolysis can be performed without exchanging devices. Since this technique was introduced, we have applied it in several acute stroke cases where there were difficulties in reopening the occluded vessels with conventional methods. The purpose of this study was to evaluate the feasibility and efficacy of the double device thrombolysis technique.
MATERIALS AND METHODS
Our institutional review board approved this retrospective study, and all patients gave written informed consent for their treatment.
From January 2008 to September 2009, 111 patients with acute ischemic stroke were treated with IAT in our institute. Among them, 20 acute stroke patients were treated by the double device technique because rapid recanalization could not be achieved with the conventional techniques that used single device or multiple devices with exchange methods. The mean age of the patients was 66 years (range 43-87). Four patients were females. The occlusion sites were as follows : middle cerebral artery (n=12; 60%), internal carotid artery terminus (ICAT) (n=5; 25%), and basilar artery (n=3; 15%).
IAT criteria and procedure
IAT was indicated when the following conditions occurred : 1) large cerebral artery occlusion, 2) 3-8 hr time window, 3) no intracranial hemorrhage, 4) perfusion-diffusion mismatching on magnetic resonance (MR) imaging, 5) initial National Institute of Health Stroke Scale (NIHSS) Ōēź4, 6) no response to intravenous tissue plasminogen activator (IVtPA) if IVtPA is indicated. Endovascular procedures were performed through a femoral artery under local anesthesia occasionally with the aid of sedative agents (midazolam and propofol). A biplane angiography unit (Integris Allura 12/12 : PHILIPS, Netherlands) was used. No heparin was given during the procedure.
We routinely inserted 8 Fr or 9 Fr femoral sheaths in order to introduce a large guiding catheter (6 Fr or 7 Fr Shuttle, Cook, USA). The large stable guiding catheter system was chosen in most of our IAT cases because large and stiff devices such as carotid and coronary stents and balloons are frequently used and so many older patients with acute stroke have tortuous aorta and neck vessels.
After placing the femoral sheath with a conventional 5 Fr catheter, cerebral angiography (both internal carotid artery and at least one vertebral artery) was obtained first in order to evaluate collateral flow and visualize the occlusion site. Once the occluded vessel was detected, a microcatheter was advanced first and superselective angiography was performed in order to see the whole thrombus burden.
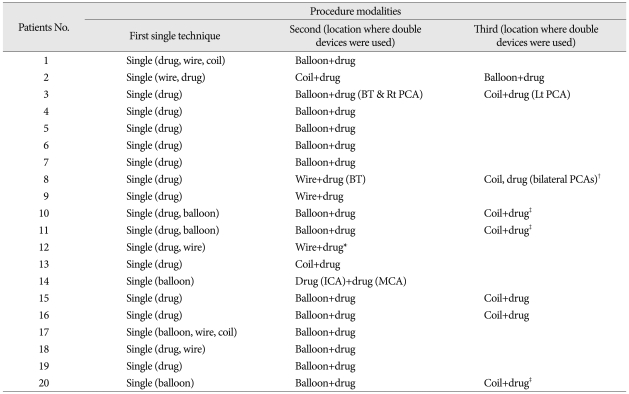
Conventional thrombolytic methods including repeated passage of soft wires and microcatheters, local infusion of thrombolytic agents, and angioplasty with balloons were tried first. When the conventional methods were not successful, the double device technique was used. In the majority of the cases, a microcatheter (excelsior SL 10; Boston Scientific, USA) and one other device was placed at the lesion site. While drugs (urokinase and/or GPIIbIIIa antagonists) were infused through the microcatheter, mechanical thrombolysis was performed at the same time using microwires, coils (GDC-soft SR 2├Ś6 mm : Boston Scientific, USA), balloons (Hyperglide : ev3, USA, or various coronary balloons), or stents (Enterprise : Cordis, USA and various coronary stents). Sometimes two occluded branches were managed simultaneously with the two devices ( Fig. 1, 2). Recanalization was assessed by a thrombolysis in cerebral infarction (TICI) grading system 5). Recanalization was established with TICI grades Ōēź2 7,11) while complete recanalization occurred with the TICI grades of 2B and 3. Follow up brain computed tomography (CT) or brain MR imaging was performed within 24 hours after thrombolysis. Symptomatic hemorrhage was defined as hemorrhage observed on follow up imaging with associated neurological deterioration Ōēź4 points according to NIHSS. Functional disability was then assessed by modified Rankin Scale (mRS). Clinical outcome was checked by mRS at 90 days. Good clinical outcome was defined as mRS Ōēż2 at 90 days. Neurological status was evaluated by stroke neurologists (HJB and MGH).
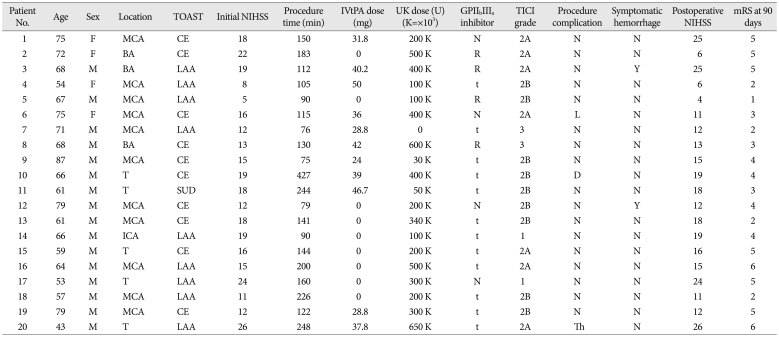
RESULTS
The clinical and neuroradiological characteristics and kinds of devices used for the double device technique are summarized in Tables 1 and 2. The median initial NIHSS was 16 (range 5-26). Patients in the combined group (n=8) received IVtPA (0.6 mg/kg) before IAT and the patients in the IAT only group (n=12) received IAT only. The overall median intra-arterial urokinase dose was 250000┬▒1900 U (range 0-700000). Median urokinase doses were 200000┬▒2300 U (range 100000-700000) and 320000┬▒1900 U (range 0-650000) in the IAT only and combined groups, respectively. In one case, no thrombolytic agents were used.
The median interval of time to treatment from stroke onset to thrombolysis therapy was 100┬▒35.6 minutes (range 70-210). The median thrombolytic procedure time from femoral artery puncture to finishing of procedure was 135┬▒83.7 minutes (range 75-427).
Any grade of recanalization was achieved in 18 patients (90%) and among them, 11 were complete recanalizations (TICI 2B in 9, TICI 3 in 2). Three procedure-related complications developed in 3 patients : iatrogenic carotid dissection, cerebral artery (M2) perforation and thrombi at the ophthalmic artery. The carotid dissection was successfully treated with a stent. Blood leakage from the M2 perforation was controlled with a temporary M2 occlusion with platinum coils. The ophthalmic artery thrombus was resolved by infusion of a thrombolytic agent. Recovery from these complications was confirmed by follow-up angiograms.
Post-procedural hemorrhage was detected on CT in five patients (25%). Of these, 2 patients (10%) were symptomatic. One patient, who had a cerebellar hemorrhage, underwent decompressive surgery because of brain stem compression and had a mRS at 90 days of 5. The other patient received conservative management and had a mRS at 90 days of 4.
Five patients (25%) had good long term outcomes with mRS scores Ōēż2 at 90 days after procedure. In two patients (10%), mortality caused by a massive infarction and associated brain edema occurred within 90 days after the procedure.
DISCUSSION
For treatment of acute stroke cases, a variety of IAT techniques have been proposed in those cases refractory to simple thrombolysis 1,8,14). However, the efficacy of a single method has often been unsatisfactory. In our experience, chemical thrombolysis alone has rarely been successful. Mechanical thrombolysis, which offers advantages in terms of efficacy and safety of IAT, is often not able to reopen the occluded vessels when performed as a single mechanical technique using a single device. Also, unlike previous study 3), for several months after the original Penumbra-system was introduced to us, we used it according to the original method for the Penumbra-system for several patients with acute ischemic stroke but we could not see the advantage to the Penumbra-system. Therefore, in real practice, there is a need to introduce the simultaneuous use of several thrombolytic devices including microcatheters and mechanical devices during IAT and sometimes, different devices are often required than that being used. If a mechanical device is needed, the microcatheter is withdrawn and the new device is introduced. If the local infusion of thrombolytic agents is needed, the mechanical device is exchanged again with a microcatheter. Practically, exchanging devices during IAT is not always a simple task and in many cases, it is technically difficult, time consuming and risky as well. Other risks include the fact that patients with acute stroke are usually old and their carotid-vertebral artery system are often tortuous and the treatment time window for these patients is usually short. In addition, in some cases when neurointerventionists need to deal with two different occlusion sites at the same time such as two M2 branches in cases of distal M1 occlusion and both P1 in cases of basilar top occlusion. The double device technique introduced in this paper was designed to allow rapid and effective recanalization in such situations as those described above. The recanalization rate of 90% that is possible with the present technique is favorable compared with previously published results (3, 11). Of note, all of our cases were refractory to conventional IAT.
In our series, procedural complications did occur in three cases. The small number of cases that made up our series does not clearly represent the real population risks and the number of complications that we observed is high compared to another study 13). This could be due to the fact that 2 of the 3 cases with complications occurred in ICAT occlusion cases. ICAT occlusions are known to be difficult lesions to reopen and these occlusions often need aggressive thrombolytic techniques 2,8,9). The overall hemorrhagic rate in our study was 25% with the symptomatic hemorrhagic rate being 10%. This rate is similar to results seen in previous trials of stroke cohorts 4,13). Again, of note, all of our cases were refractory to conventional IAT. The median procedural time in our study was 2.25 hours. This time is similar to previous studies with conventional methods 4,13). However, it is important to consider that the double device technique in our series was performed only in cases refractory to conventional thrombolysis and the procedural time in our study includes the time of conventional thrombolysis. The prominent advantage of the double device thrombolysis technique is the practical easiness. The conditions of the lesion site changes as thrombolysis progresses. If one microcatheter is present at the lesion with a mechanical device manipulated, we can figure the changes anytime by selective angiograms without exchanging devices. Thrombolytic agents can be locally infused simultaneously with mechanical thrombolysis. Proximal and distal parts of the occluding thrombi can also be dissolved at the same time and two distal occluded vessels can be managed together. These simultaneous procedures are often necessary when the time window is thisclose. Thus, we have shown that we can reduce procedural times and the frequency of device exchange during IAT.
The limitations of this study include it being a retrospective analysis, that it occurred at a single institute, and in the small number of cases. It is obvious that larger prospective, multi-institutional studies are necessary to prove the feasibility and safety of this technique. However, our study suggests that a double device technique might be useful for intractable large vessel occlusions not treatable by conventional techniques.
CONCLUSION
The double device thrombolysis technique is a feasible and effective technical option of IAT for acute stroke cases which are refractory to conventional thrombolysis.
References
1. Abou-Chebl A, Bajzer CT, Krieger DW, Furlan AJ, Yadav JS : Multimodal therapy for the treatment of severe ischemic stroke combining GPIIb/IIIa antagonists and angioplasty after failure of thrombolysis. Stroke 2005, 36 : 2286-2288,   2. Arnold M, Nedeltchev K, Mattle HP, Loher TJ, Stepper F, Schroth G, et al : Intra-arterial thrombolysis in 24 consecutive patients with internal carotid artery T occlusions. J Neurol Neurosurg Psychiatry 2003, 74 : 739-742,    3. Bose A, Henkes H, Alfke K, Reith W, Mayer TE, Berlis A, et al : The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol 2008, 29 : 1409-1413,    4. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al : Prolyse in Acute Cerebral ThromboembolismIntra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. JAMA 1999, 282 : 2003-2011,   5. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al : Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 2003, 34 : e109-e137,   6. Kim DJ, Kim DI, Byun JS, Jung JY, Suh SH, Kim EY, et al : Simple microwire and microcatheter mechanical thrombolysis with adjuvant intraarterial urokinase for treatment of hyperacute ischemic stroke patients. Acta Radiol 2008, 49 : 351-357,   7. Levy EI, Mehta R, Gupta R, Hanel RA, Chamczuk AJ, Fiorella D, et al : Self-expanding stents for recanalization of acute cerebrovascular occlusions. AJNR Am J Neuroradiol 2007, 28 : 816-822,   8. Lin R, Vora N, Zaidi S, Aleu A, Jankowitz B, Thomas A, et al : Mechanical approaches combined with intra-arterial pharmacological therapy are associated with higher recanalization rates than either intervention alone in revascularization of acute carotid terminus occlusion. Stroke 2009, 40 : 2092-2097,   9. Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, et al : Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke 2002, 33 : 2066-2071,   10. Nakano S, Iseda T, Yoneyama T, Kawano H, Wakisaka S : Direct percutaneous transluminal angioplasty for acute middle cerebral artery trunk occlusion : an alternative option to intra-arterial thrombolysis. Stroke 2002, 33 : 2872-2876,   11. Nogueira RG, Schwamm LH, Buonanno FS, Koroshetz WJ, Yoo AJ, Rabinov JD, et al : Low-pressure balloon angioplasty with adjuvant pharmacological therapy in patients with acute ischemic stroke caused by intracranial arterial occlusions. Neuroradiology 2008, 50 : 331-340,   12. Qureshi AI, Siddiqui AM, Suri MF, Kim SH, Ali Z, Yahia AM, et al : Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery 2002, 51 : 1319-1327; discussion 1327-1329,   13. Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al : Mechanical thrombectomy for acute ischemic stroke : final results of the Multi MERCI trial. Stroke 2008, 39 : 1205-1212,   14. Yoon W, Park MS, Cho KH : Low-dose intra-arterial urokinase and aggressive mechanical clot disruption for acute ischemic stroke after failure of intravenous thrombolysis. AJNR Am J Neuroradiol 2010, 31 : 161-164,   
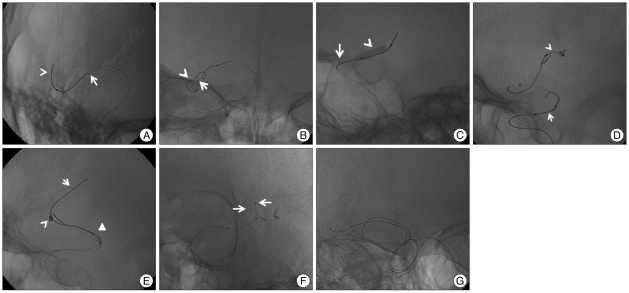
Fig.┬Ā1
We performed a double device technique for efficient thrombolysis with a combination of various devices such as the following : combination wire (arrowhead) with catheter (white arrow) (A), coil (arrowhead) with catheter (white arrow) (B), balloon (arrowhead) with catheter (white arrow) (C), coil (arrowhead) with balloon (white arrow) (D), and coil (arrowhead) with wire (white arrow) through stent (triangle) (E). In addition, we used two devices at different occlusion sites for simultaneous thrombolysis with the following : microcatheter and microcatheter (F) and microwire and microwire (G). 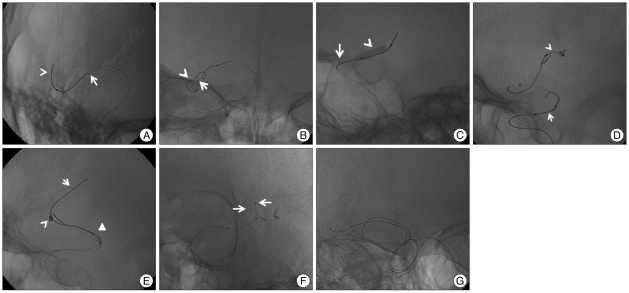
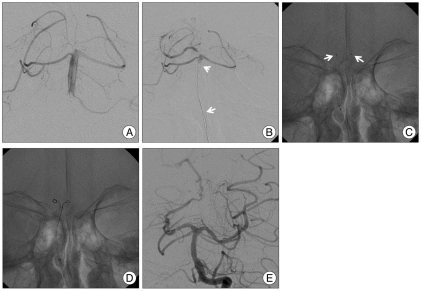
Fig.┬Ā2
A : Selective angiogram showing occlusion at BT and bilateral PCAs. B : Angiogram obtained during thrombolysis with the double device technique (arrowhead : wire, white arrow : microcatheter) showing occlusion at the proximal portion of the right PCA and left PCA. C : Two microcatheters (white arrow) were placed at proximal portions of different PCAs. D : Thrombolysis was performed by the double device technique with coils at bilateral PCAs. E : Final angiogram showing complete recanalization. BT : basilar tip, PCAs : posterior cerebral arteries. 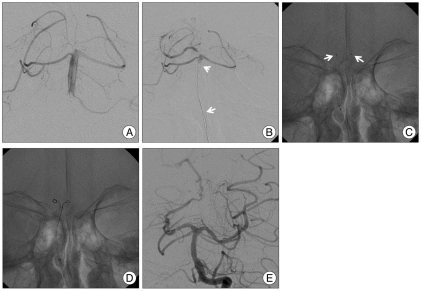
Table┬Ā1
Summary of the characteristics of the patients, procedural results, and occlusion location 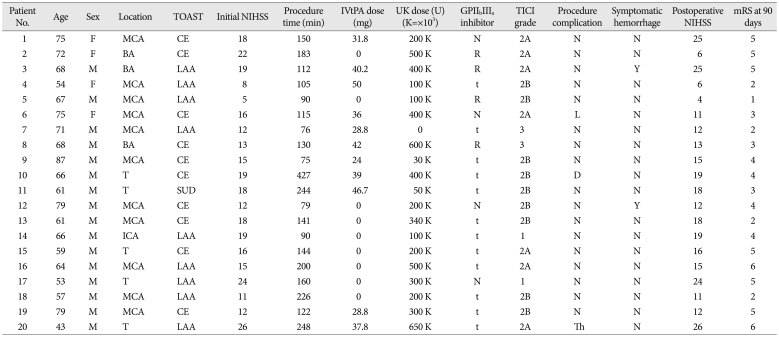
Table┬Ā2
Devices used and procedure modality of each patient 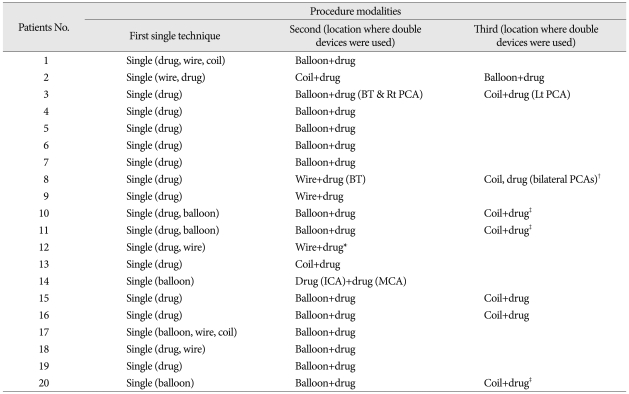
|
|